In the 19th century, Claude Bernard, the father of evidence-based medicine, first noted that the Vagus nerve was a structural and functional link connecting heart and brain. It has been several decades since the concept of “vagal atrial fibrillation (AF)” was proposed, implicating parasympathetic activation as a contributor to initiation and perpetuation of AF 1. Although, pulmonary vein isolation (PVI) remains the cornerstone for ablation in patients with paroxysmal AF, the autonomic nervous system (ANS) may be one of the contributors 2.
In the autonomic nervous system (ANS), the ganglion cells of the autonomic nerves are divided into extrinsic (outside the heart) and intrinsic (inside the heart) parts. While the extrinsic part of the vagosympathetic system is located in the brain and spinal cord, the intrinsic part includes ganglionated plexuses (GPs) on the epicardial surface of the left and right atria and in the ligament of Marshall 3-5. The GP contain afferent sensory neurons from the atrial myocardium, efferent parasympathetic and sympathetic neurons (with heavy innervation of the pulmonary vein myocardium and the atrial myocardium surrounding the GP), and local interconnecting neurons. These interconnecting neurons cause a communication network between the different GPs and between the GP and other parts of the atrium 6-8.
Considering the possible role of the ANS in the initiation and maintenance of AF, modulation of ANS by GP ablation has emerged as a method to improve outcomes. The first GP mapping technique for AF treatment was described by Pachon et al 9 in 2004. Here, we aimed to discuss the current data on the role of the GPs in the pathogenesis of AF and potential therapeutic implications.
Anatomical localization of ganglionated plexuses
The intrinsic cardiac ANS contains clusters of autonomic ganglia located in epicardial fat pads and in the ligament of Marshall. Armour et al 4 called these clusters as GPs. Following 5 major atrial locations were consistently identified in great majority of cases: (1) the superior surface of the right atrium (superior right GP); (2) the superior surface of the left atrium (superior left GP), (3) the posterior surface of the right atrium (inferior right GP), (4) the posterior medial surface of the left atrium (posteromedial left GP), and (5) the inferolateral aspect of the posterior left atrium (posterolateral left or left inferior GP). Pauza et al 5 described slightly different anatomic distribution for GPs in another human anatomical study. However, both agree that the great majority of neuronal bodies are concentrated within the posterior right atrial GP and the posteromedial left atrial GP Figure 1.
Figure 1. The location of ganglionated plexuses (GPs) and circumferential PVI in atrial electro-anatomic maps. GPs sites are shown as green dots and PVI are shown as red dots.
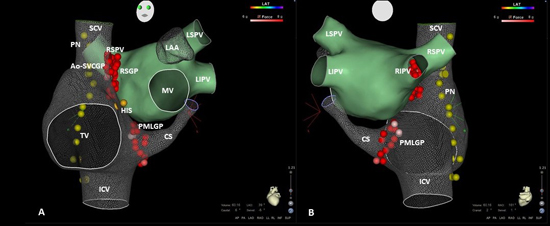
A-B, LSGP, LIGP, RSGP and RIGP distribute in the left atrium near LSPV, LIPV, RSPV and RIPV, respectively. LAA, left atrial appendage; LIGP, left inferior GP; LSGP, left superior GP; RSGP, right superior GP; RIGP, right inferior GP; MV, mitral valve; PVI, pulmonary vein isolation
By using Fast Fourier Transform analysis, Pachon et al 9 defined two types of atrial myocardium: (1) compact atrial myocardium demonstrates uniform and fast conduction properties and (2) fibrillar atrial myocardium demonstrates fragmented and heterogeneous conduction properties. Fibrillar potentials were usually found in the atrial wall near the pulmonary vein insertions, in the interatrial septum, and in the junction of superior vena cava and right atrium. Thus, they claimed that fibrillar potentials may be used to detect localization of GPs during electrophysiological study.
High frequency stimulation (HFS) with different protocols have been used to localize GPs for a long time by different groups 10-14. GP stimulation results in both sympathetic and parasympathetic activity, but parasympathetic reflexes are almost immediate. Therefore, a positive vagal response during HFS application which is defined as an increase of PP or PR interval during sinus rhythm or a >50% increase in mean R-R interval during AF is used to detect localization of GP. According to HFS response, Po et al 15 described 4 GPs in the left atrium: (1) superior left GP (on the roof of the left atrium, near the medial side of the left superior pulmonary vein); (2) anterior right GP (located anterior to the right superior pulmonary vein); (3) inferior left GP (at the inferior aspect of the posterior left atrial wall); and (4) inferior right GP (just below the left and right inferior pulmonary veins).
Although GPs contain both efferent cholinergic and adrenergic neurons, in the sympathetic nervous system, great majority of postganglionic neurons are located in paravertebral ganglia 3. On contrary, the axons of presynaptic parasympathetic neurons extend from the central nervous system into GPs. As a result, the postsynaptic parasympathetic nerve fibers are very short. Theoretically, if the locations of GPs can be detected during electrophysiological study, radiofrequency ablation on these sites will damage both neuronal bodies and nerve fibers in the parasympathetic system but will mainly affect nerve fibers in the sympathetic system. Based on these anatomical relationships, GP ablation was considered to allow selective vagal denervation while sympathetic and sensory neurons are preserved. However, GP ablation techniques aim to modify the behavior of the cardiac ANS to prevent some/all of the autonomic processes occurring in AF.
Electrophysiological effects of ganglionated plexuses
Dysregulation of the ANS in favor of parasympathetic over-activity, which may also occur because of sympathetic withdrawal, often result in significant bradyarrhythmia episodes such as vasovagal syncope, sinus bradycardia, and functional atrioventricular block 16. Clinical evidence for potential role of vagal activity in human AF has been provided by observations of Coumel 17 and Chen et al 18. Stimulation of cervical vagal trunk has for decades been used for the induction and maintenance of AF in experimental protocols 19,20.
According to previous experimental studies, parasympathetic stimulation shortens the atrial effective refractory period (AERP), thereby decreasing the wavelength of atrial excitation wave fronts 20-22. The shorter wavelength increases the probability that multiple reentrant circuits can exist simultaneously in the atrial myocardium by expanding window of vulnerability and then increases the stability of AF. Vagal stimulation may also increase AERP heterogeneity in different atrial sites 10. Furthermore, while local application of acetylcholine around GPs caused a similar atrial electrophysiological substrate changes and AF-triggering effect as described above, this relationship was eliminated by blocking vagus nerve function with drugs such as atropine 12,13. However, the interpretation of these findings is controversial because the concomitant release of adrenergic neurotransmitters may also mobilize excess calcium intracellularly leading to early after depolarizations and triggered firing particularly in pulmonary vein myocytes 23. It is well known that that, pulmonary vein myocytes have a shorter action potential duration and a greater sensitivity to both cholinergic and adrenergic stimulation than adjacent atrial tissue, which may explain why AF usually start with an extra beat arising from pulmonary veins. 12,13,23. To define the mechanism how a single pulmonary vein depolarization is converted to AF, Scherlag et al 12 investigated the effects of GP stimulation at voltages ranging from 0.6 to 4.0 V in 14 anesthetized dogs. They demonstrated that, stimuli applied to pulmonary veins would not induce AF unless there was simultaneous stimulation of the adjacent GP (20 Hz, 0.1-ms pulse width) that excites the atrial myocardium. Same group showed that, muscarinic receptor blockade prevented action potential duration shortening and focal firing originating from the adjacent PV 13. Furthermore, Chen et al 24 demonstrated that, activation of intrinsic cardiac ANS is observed prior to the onset of paroxysmal AF in nearly 100% cases, where 20% suffered the attack in the absence of extrinsic cardiac ANS afferent signals, suggesting that intrinsic part or GPs could trigger AF completely independently of extrinsic one.
The main contribution of this experimental data in a clinical perspective is that it led to establishment of a novel technique for GP mapping and ablation.
The role of percutaneous ganglionated plexus ablation alone strategy on atrial fibrillation treatment.
As it has been shown that, the ANS plays a important role in initiating AF and in atrial autonomic remodeling, neuromodulation through GP ablation, either alone or in combination with PVI, has been investigated.
In the first human study, Pappone et al. 25 evaluated the potential role of GP ablation by RF in preventing recurrent AF in patients undergoing circumferential pulmonary vein ablation for paroxysmal AF. During ablation, the sites demonstrating positive vagal response were identified and ablated until either these reflexes were abolished. The abolition of all vagal reflexes was defined as complete vagal denervation and obtained in 34.3% of the 297 paroxysmal AF patients. Late AF recurrences were less frequent in vagal denervation group. However, GPs were not specifically targeted in any patient.
By using HFS to detect GPs, in a population of 63 patients with paroxysmal AF undergoing left atrial GP ablation followed by PVI, GP ablation alone (prior to PVI) decreased the occurrence of pulmonary vein firing (without isoproterenol or other stimulants) from 47 (75%) of 63 patients before GP ablation to only 9 (14%) of 63 patients (P<0.01) after GP ablation 26. By using Fast Fourier transform analysis, ablation of fibrillar myocardium without PVI was found related to 94% freedom from AF after follow-up of 9.9 ± 5 months 9.
In a small population of selected patients presenting episodes suggestive of vagal-induced paroxysmal AF and no heart disease, Scanavacca et al 27 compared GP ablation alone and PVI alone strategies. The target atrial GPs had been detected based on the anatomical description of Armour et al 4 and it mainly involved GPs around the pulmonary veins. After a mean follow-up of 8.3±2.8 months, just 2 of 10 patients in the ‘denervation group” were free from recurrences (although all of them have presented heart rate variability compatible with vagal modification), whereas all patients receiving PVI alone remained in sinus rhythm. Similar results were obtained by Katritsis et al 28 comparing GP ablation alone to PVI: AF recurring in 37% of patients with circumferential ablation and 74% of those with GP ablation (p=0,017), during 1-year follow-up. On contrary, in the following work of the same group, HFS-based GP ablation was compared with extensive empirical GP ablation in patients with paroxysmal AF 14. At 13.1 ± 1.9 months, 42.5% of patients with HFS-based GP ablation group and 77.5% of patients with anatomic ablation group were free of symptomatic paroxysmal AF. Furthermore, the decrease in heart rate variability parameters demonstrating parasympathetic tone were significantly higher in the empirical ablation group. The use of selective GP ablation were independent predictors of recurrent AF. Authors concluded that, selective GP ablation directed by HFS is inferior to extensive, regional ablation at the presumed anatomic sites of the plexi.
According to evidence as mentioned above, GP ablation alone strategy should not be considered as alternative to PVI at this time. Methodology of GP detection may be the cause of conflicting results.
Percutaneous ganglionated plexus ablation in addition to pulmonary vein isolation
PVI may inadvertently ablate the GP but this response is not identical between patients due to anatomical settlement of GPs 29. In the clinical study of Pappone et al 25, vagal denervation was defined as abolition of all evoked vagal reflexes during radiofrequency application. Although, 99% of patients with vagal reflexes were free of symptomatic AF, by using this definition, authors obtained a “complete vagal denervation” in only 34.3% of patients. Given that it was a non-randomized observation, the evidence that adjunctive denervation is effective has limited strength. However following studies and meta-analyses have demonstrated the feasibility and effectiveness of GP ablation plus PVI in this population 30-36Table 1.
Table 1. Summary of clinical studies regarding ganglionatedplexi ablation in patients with atrial fibrillation.
| Study |
Year |
Approach |
Ablation sites |
Desing group |
AF tipes |
Number of patients |
Outcomes |
| Pachon |
2004 |
Nest whitout PVI |
Endocardial |
Observational study |
Paroxysmal and persistent |
40 |
AF free survival: 94% |
| Pappone |
2004 |
CVD+PVI |
Endocardial |
Observational study |
Paroxysmal |
297 |
CVD in 34.3%.
Late AF
recurrence were
less frequent |
| Scherlag |
2005 |
GP+PVI vs
PVI |
Endocardial |
Unknown |
Paroxysmal or
persistent |
60 |
AF free
survival: 91%
in GP+PVI
group vc 71%
in PVI group |
| Scanavacca |
2006 |
GP ablation
vs PVI |
Epicardial
and/or
endocardial |
Observational
Study |
Paroxysmal |
10 |
Recurrence in
5/7 patients
who underwent
denervation |
| Katritsis |
2008 |
GP vs CPVI |
Endocardial |
Case- controlled
study |
Paroxysmal |
38 |
AF recurrence:
74% (GP
ablation group)
vs 37% (PVI
group)
(p=0.017) |
| Po |
2009 |
GP+PVI |
Endocardial |
Observational
Study |
Paroxysmal and
persistent |
80 |
Free of AF/AT
after a single
ablation: 80% at
12 months |
| Pokushalov |
2009 |
Selective GP
vs anatomic
GP ablation |
Endocardial |
Observational
study |
Paroxysmal and
persistent |
80 |
Free of
paroxysmal AF:
42.5% in
selective GP
ablation vs
77.5% in
anatomic GP
ablation
(p=0.02) |
| Pokushalov |
2010 |
Anatomic
GP |
Endocardial |
Observational
study |
Paroxysmal |
56 |
AF free survival
at 12 months:
71% |
| Mikahylov |
2011 |
GP vs CPVI |
Endocardial |
Case- controlled
study |
Paroxysmal |
70 |
AF/AT Free
survival: 34.3%
(GP ablation
group vs 65.7%
(PVI group)
(p=0.008) |
| Katritsis |
2011 |
GP+PVI vs
PVI |
Endocardial |
RCT |
Paroxysmal |
67 |
Arrhythmia (AF
or AT) free
survival: 85.3%
in PVI+GP
group vs 60.6%
in PVI group
(p=0.019) |
| Katritsis |
2013 |
GP+PVI vs
GP vs PVI |
Endocardial |
RCT |
Paroxysmal |
242 |
AF free
survival: 74%
(GP+PVI) vs
48% (GP) vs
56% (PVI)
(p=0.004) |
| Pokushalov |
2013 |
PVI+GP vs
PVI+LL |
Endocardial |
RCT |
Persistent |
264 |
AF free
survival: 47%
PVI+LL vs
54% (PVI+GP)
(p=0.29) |
| Driesgen |
2016 |
PVI vs
PVI+GP
(Dallas
lesion if
persistent
AF) |
Thoracoscopic |
RCT |
Paroxysmal and
persistente |
240 |
Freedom from
AF:70.9% vs
68,4%
(p=0.696) |
| Steinberg |
2020 |
PVI vs
PVI+RDN |
Endocardial |
RCT |
Paroxysmal |
302 |
Freedom from
AF/AT: 56,5%
in PVI vs
72,1% in
PVI+RDN
(p=0.006) |
AT, atrial tachycardia. Please see text for other abbreviations
Katritsis et al 30 compared GP ablation + PVI with PVI alone for treatment of paroxysmal AF. Sixty-seven patients with paroxysmal AF were randomized. At the end of follow-up, 20 (60.6%) patients in the PVI group and 29 (85.3%) patients in the GP+PVI group remained arrhythmia-free (log rank test, P = 0.019).
In a randomized study, a total of 242 patients with symptomatic paroxsysmal AF were recruited and randomized as follows 35: 1) circumferential PVI (n = 78); 2) anatomic ablation of the main left atrial GPs (n = 82); or 3) circumferential PVI followed by anatomic ablation of the main left atrial GPs (n = 82). Freedom from AF or AT was achieved in 44 (56%), 39 (48%), and 61 (74%) patients in the PVI, GP, and PVI+GP groups, respectively (p = 0.004 by log-rank test). PVI+GP ablation strategy compared with PVI alone yielded a hazard ratio of 0.53 (95% confidence interval: 0.31 to 0.91; p = 0.022) for recurrence of AF or atrial tachycardia.
Pokushalov et al 33 randomized 264 patients with long-lasting persistent (32%) and persistent AF (68%) to PVI+GP ablation (132 patients) and PVI+linear lesions (LL) (132 patients) groups. By using an implantable monitoring device, they identified that after 3 years, 34% of patients with PVI+LL and 49% of patients with PVI+GP ablation maintain sinus rhythm, respectively (p = 0.035). After a second procedure, long-term success was seen in 52% of the PVI + LL group and in 68% of the PVI + GP group, respectively (p = 0.006). As a main limitation of the study, techniques were not compared with PVI alone strategy.
In a recently published meta-analysis, of 4 randomized control trials with 718 patients, GP ablation plus PVI was compared with PVI alone strategy according to the AF subtype 36. Among paroxysmal AF patients, GP ablation was linked to significantly higher freedom from atrial tachycardia/AF (75.8 vs. 60.0%, respectively; OR 95% CI: 2.22 1.36– 3.61, P = 0.001). Among persistent AF patients, GP ablation was associated with a non-significant trend towards higher rates of freedom from atrial tachycardia /AF (54.7 vs. 43.3% for the intervention vs. control arms respectively; OR 95% CI: 1.55 0.96–2.52, P = 0.08).
In another meta-analysis, Qin et al 31 evaluated the efficacy of adjunctive GP and complex fractionated atrial electrogram (CFAE) ablation strategies by systematic review of randomized clinical trials and non- randomized clinical trials. In subgroup analysis, addition of GP ablation increased rates of freedom from atrial tachyarrhythmia (1.72 1.21, 2.45; P = 0.003). Overall, the pooled estimate showed that compared to PVI, adjunctive GP/CFAE ablation further increased long-term sinus rhythm maintenance (1.90 1.37, 2.63; P = 0.0001), without significant heterogeneity among included studies. Subgroup analysis showed better sinus rhythm maintenance in favor of GP/CFAE plus PVI, with the difference being statistically significant only for adjunctive GP ablation (2.0 1.34, 2.98; P = 0.0006).
In studies investigating role of GP ablation on AF, operators presumed that GPs are located around the PVs 37. So, they targeted the sites around the PV ostium. However, according to human autopsy-based anatomical studies, the largest number of GPs are located in the posterior surface of the right atrium adjacent to the interatrial groove, and these GPs contain much more neurons compared with the others 3,4. Thus, PV based approaches may not be enough for vagal denervation and more selective definition localization of GPs during electrophysiological study may improve the results 38,39. A possible lesion set for a more limited ablation targeting exclusively inter-atrial septum GPs to avoid larger scar tissue is provided in Figure 2.
Figure 2. The location of septal ganglionated plexuses (GPs) in atrial electro-anatomic maps. GPs sites are shown as red dots.
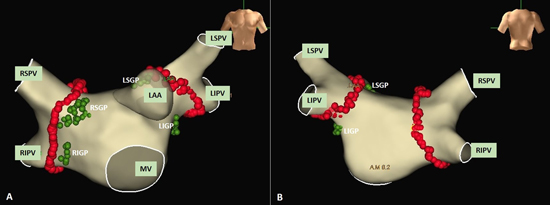
A-B: RSGP distribute in the anterior left atrium near RSPV, PMLGP distribute in the posterior left atrium near ostium CS and Ao-SVC GP located between the medial superior vena cava and aortic root.
Surgical ganglionated plexus ablation
Although the third version of Cox-Maze procedure is considered the gold standard surgical procedure for AF, it cannot be applied for the treatment of lone AF due to its invasiveness and complexity 40. Recently, minimally invasive surgery has been reported as a reasonable option for patients with lone AF based on the benefit of a smaller incision and reduced complications related to cardiopulmonary bypass as compared to Cox-Maze surgery. Theoretically, surgical GP ablation may cause more complete GP ablation than endocardial catheter ablation considering sub-epicardial clustering of GPs. However, despite existence of some positive data after endocardial GP ablation, GP ablation by using minimally invasive surgery has not shown beneficial effects in preventing AF recurrence 41.
Recently, a randomized controlled study - Atrial Fibrillation Ablation and Autonomic Modulation by Thoracoscopic Surgery (AFACT) - tested the efficacy of additional GP ablation by using thoracoscopic surgery technique 42. All patients with persistent AF underwent PVI by thoracoscopy and additional linear lesions (Dallas lesion set). Two hundred and forty patients were randomized to additional GP ablation (GPs group) or PVI alone (control group). Four main GPs were located using anatomical landmarks and HFS. GP ablation completely eliminated vagal responses, while 87% in the control group still exhibited vagal responses. The GP group showed no statistically significant difference in AF recurrence compared to the control group.
There are several possible reasons to explain why previous randomized studies using catheter ablation had better results than the surgical technique: (1) the AFACT population consisted of patients with persistent AF, with dilated left atrium and previous ablations, and therefore a recurrence-prone profile and (2) approach to intra-atrial endocardial and subepicardial GPs could require dissection of anatomical pockets such as those between inferior vena cava and coronary sinus, or between the superior vena cava and right pulmonary veins, usually not performed and hardly achieved during surgery but still accessible by endocardial RF ablation. Histological sections of those regions reveal fat pads containing numerous well-formed encapsulated autonomic ganglia 43.
The lack of confirmation of immediate and late cardiac denervation effect after GP ablation procedures is another critical issue that could be responsible for poor results in some studies. Elimination of positive vagal response to high frequency stimulation in any site which demonstrated positive response in the pre-ablation attempt might be a surrogate and probably one of the most broadly used endpoint in clinical studies 30,32,34,36,44-47.On the other hand, hard immediate end points such as significant enhancement of the sinoatrial and atrioventricular node functions verified during EP study, a negative response to atropine test and abolition of bradycardia induced by extra-cardiac vagus nerve stimulation after endocardial GP ablation have being preferred in recent works 48-55. Equally important, heart rate variability parameters demonstrating parasympathetic tone such as RMSSD, pNN>50 may be used to detect possible autonomic tone recovery. In fact, late vagal tone recovery after denervation with different techniques is a well-demonstrated technical limitation that could be responsible for a significant part of arrhythmia recurrences 49-51,54.
Functional autonomic recovery after GP ablation has been associated with terminal fibers regeneration (parasympathetic reinnervation). Furthermore, a supersensitive response to acetylcholine in the long term may imply an increased number or density of muscarinic receptors after GP ablation as another cause of vagal tonus recovery 56.
Role of renal sympathetic denervation in atrial fibrillation
Renal sympathetic denervation (RDN) is emerging as a novel approach for treatment of patients with resistant hypertension 57. Comprehensive autonomic modification can be provided by RDN, reducing cardiac sympathetic nerve activity and the reno-cardiac axis, resulting in possibly better outcomes in patients with AF. There is no clinical data available on the role of RDN as a lone approach to AF.
Significant data have been provided in the last few years on the role of RDN added to the conventional approach for AF treatment. One of the early studies was a meta-analysis performed by Pokushalov et al 58 comparing the role of RDN as an adjunct to PVI in patients with AF and moderate or severe resistant hypertension from 2 different prospective randomized studies. After 12 months of follow up, 63% of patients in the combined approach and 41% of patients in the PVI only group were free from recurrences (p=0.014). With a similar methodology, Romanov et al 59 compared the effect of PVI-only or PVI+RDN in patients with paroxysmal or persistent AF and resistant hypertension. By using an implantable cardiac monitor, AF episodes, AF burden and blood pressure were compared between groups. The combined approach was found to be superior. Authors concluded that, renal artery denervation added to PVI could have a significant role in the management of AF.
A randomized prospective study has recently confirmed these findings and again demonstrated that RDN in addition to PVI rendered better clinical results compared with catheter ablation alone strategy in patients with paroxysmal AF and hypertension 44. A recent meta-analysis comprising of six randomized controlled studies including 689 patients with hypertension and symptomatic AF demonstrated that, RDN+PVI (387 patients with irrigated radio-frequency catheters and 302 with cryoballoon) conferred better results compared with PVI alone after 12 months of follow-up (mean odds ratio for AF recurrence was 0.43; 95% confidence interval 0.32-0.59 45).
Finally, RDN+PVI strategy had a valuable role in a subset of patients with AF and chronic kidney disease (CKD), with freedom from AF recurrences being achieved in 65.5 in RDN+PVI group vs 38,5% in patients with PVI alone group, respectively (p=0,02). Furthermore, the greater benefit was observed among patients with CKD stage 4.