Cardiothoracic Surgery Residency Training in Surgical Ablation for Atrial Fibrillation
Zachary M. DeBoard1,2, Thomas K. Varghese Jr 2, John R. Doty 3, Craig H. Selzman2
1Division of Cardiac & Thoracic Surgery, Providence Regional Medical Center Everett, Everett, WA.2Division of Cardiothoracic Surgery, University of Utah, Salt Lake City, UT.3Division of Cardiothoracic Surgery, Intermountain Medical Center, Murray, UT.
As no standardized curriculum exists for training cardiothoracic surgery residents in surgical ablation for atrial fibrillation there is potential for variation in operative technique, patient selection, and overall application. Thus we sought to assess the exposure of current residents in order to identify areas for improvement in their education.
A survey was emailed to residents inquiring about their training experience in surgical ablation for atrial fibrillation. Residents were asked about case volume, procedural variety, and guideline-based clinical scenarios where they felt ablation would be appropriate. Residents were also queried about their abilities to perform various lesion sets and overall satisfaction with training.
The respondents performed a median of five cases during training with pulmonary vein isolation the most common lesion set. Seventy seven percent of residents are unable to independently perform a bi-atrial (Cox-Maze IV) lesion set. Residents are neutral regarding their satisfaction with training in surgical ablation for atrial fibrillation.
The findings of low case volume, incomplete lesion set use, and lack of training satisfaction suggests residents are being insufficiently exposed to surgical ablation of atrial fibrillation. These findings should inform educators on the importance of a more thorough experience during training given the increasing prevalence of atrial fibrillation and the need for appropriate and durable surgical intervention.
Key Words : Atrial Fibrillation, Ablation, Surgery, Training, Residency.
Correspondence to: Zachary M. DeBoard, MD Cardiac and Thoracic Surgery Providence Regional Medical Center Everett 1330 Rockefeller Avenue Suite 400 Everett, WA 98201
Current guidelines support a broad use of concomitant and stand-alone surgical ablation for atrial fibrillation (AF).[1,2] Given the expected increase in AF prevalence and the burdens associated with its sequelae, it is conceivable that more surgeons will be tasked with performing ablations.[3,4] However, no standardized curricula exist regarding training in surgical ablation of AF. With likely substantial variation of lesion sets and the potential for indiscriminate application of surgical ablation, it remains unknown if current cardiothoracic (CT) surgical residents are receiving adequate instruction during training. The consequence of this may result in inadequate ablation techniques as well as missed opportunities for patient intervention.[5,6] Hence, we sought to better understand the current state of ablation education by evaluating current CT surgery residents’ training experience in surgical AF ablation.
The University of Utah Institutional Review Board determined this study exempt. An anonymous survey was emailed to current United States CT surgery residents in May 2018. Email addresses were obtained from the Thoracic Surgery Directors Association (TSDA) list. Senior-level residents (post graduate year six and greater) were included in the final analysis, as they were considered likely to have had significant or focused exposure to cardiac surgery and are nearing entering the workforce. The full survey with questions & response choices appears in the appendix. The total of possible respondents was based on the number of 2018 senior-level in-service examinees (n=248). Residents were excluded if their TSDA-supplied email addresses were non functional (n=36) as was the first author and other residents at the sponsoring institution (n=4). Participants were queried on training program characteristics, AF ablation/arrhythmia surgery case volume (non-pacemaker or pacemaker lead related), observed surgical approaches and lesion sets, and management strategy for the left atrial appendage. Residents were also asked about their opinion on the appropriate application of stand-alone and concomitant ablation in clinical scenarios based on recent society guidelines. Finally, residents rated their abilities to independently perform various lesion sets and their overall satisfaction with training in AF ablation via five-point Likert scales (“unable/unsatisfied, somewhat unable/unsatisfied, neutral, somewhat able/satisfied, completely able/satisfied;” numeric values: 1-5, respectively). Program names and other identifying data, such as region of the country, were not collected in this study.
Fifty-two senior residents responded yielding a response rate of 25% (52/208). Most are training at two- and three-year “traditional” residencies (n=45, 86.5%) rather than integrated programs and are pursuing a “cardiac-focused” path. Residents performed a median of five ablations (interquartile range [IQR]: 3-10) as the primary surgeon. Most trainees’ programs do not perform stand-alone ablation surgery (n= 29, 55.8%). A median sternotomy (94.2%) is the most employed approach to performing ablations with a pulmonary vein isolation (PVI) being the predominant lesion set at trainees’ programs (44.2%). A combination of cryothermy and radiofrequency are the most commonly employed energy sources for creating lesions (63.4%) and the left atrial appendage is primarily excluded via an external device ligation (57.7%). Responses to training environment characteristic questions appear in [Table 1]. The percentages of responders finding it appropriate to perform concomitant and stand-alone ablations in various guideline-based clinical scenarios appear in [Table 2].
Table 1. Survey questions & responses of the 52 senior resident participants
| Survey Question |
Respondents (n=; %) |
| What is your current post-graduate year level (PGY) of training? |
| PGY-6 |
24; 46.2 |
| PGY-7 |
20; 38.4 |
| PGY-8 |
8; 15.4 |
| In which type of training program are you enrolled? |
| Traditional 2-year |
28; 53.8 |
| Traditional 3-year |
17; 32.7 |
| Integrated or combined (I-6, 4+3) |
7; 13.5 |
| Which training track are you pursuing? |
| Cardiac |
35; 67.3 |
| Thoracic |
8; 15.4 |
| None |
9; 17.3 |
| Does your program surgical ablation of AF as a stand-alone operation? |
| No |
29; 55.8 |
| Yes |
23; 44.2 |
| Which approach does your program use to perform ablation? (select all that apply) |
| Median sternotomy |
49; 94.2 |
| Thoracoscopic |
14; 26.9 |
| Right thoracotomy |
8; 15.4 |
| Bilateral thoracotomy |
3; 5.8 |
| What is the predominant lesion set used at your program? |
| Pulmonary vein isolation |
23; 44.2 |
| Bi-atrial (full) maze |
21; 40.4 |
| Left atrial maze |
8; 15.4 |
| Which energy sources does your program use? (select all that apply) |
| Combined radiofrequency & cryothermy |
33; 63.4 |
| Cryothermy alone |
30; 57.7 |
| Radiofrequency alone |
20; 38.5 |
| Cut and sew |
4; 7.7 |
| How does your program manage the left atrial appendage? |
| External ligation/device |
30; 57.7 |
| Excision and oversewing |
13; 25.0 |
| Internal (intra-atrial) suture closure |
7; 13.5 |
| Stapling |
2; 3.8 |
Table 2. Scenarios in which survey respondents would perform surgical ablation of AF
| Scenario |
Percentage of
respondents (n=52) |
| Concomitant operation |
| Mitral valve repair/replacement |
98 % |
| Coronary artery bypass & valve replacement |
90.4 % |
| Tricuspid valve repair/replacement |
88.5 % |
| Coronary artery bypass |
84.6 % |
| Aortic valve replacement |
77.5 % |
| For postoperative AF prophylaxis |
19.2 % |
| Repair of aortic dissection |
17.3 % |
| Stand-alone ablation |
| Symptomatic from arrhythmia |
98 % |
| Failed catheter ablation |
86.5 % |
| Refractory to anti-arrhythmic drug(s) |
86.5 % |
| Contraindication to/intolerant of anticoagulation |
82.7 % |
| Combined with catheter ablation (hybrid approach) |
48.1 % |
| Asymptomatic but with long-standing persistent AF |
17.3 % |
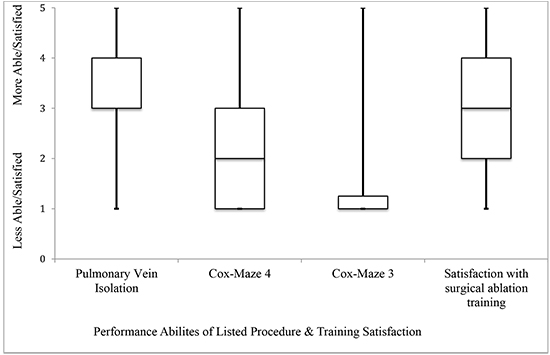
Residents stated they are “somewhat able” (median: 4, IQR: 3-4) to independently perform PVI. The majority of residents (86.5%, n=45) stated they are unable to independently perform a bi-atrial Cox Maze (CM) III or IV (median: 1, IQR: 1-1.25; median: 2, IQR: 1-3, respectively). Finally, residents stated they are “neutral” (median: 3, IQR 2-4) with regard to their satisfaction in surgical AF ablation training. Procedural ability and training satisfaction results appear graphically in [Figure 1]
Figure 1. Box plot of the survey responders’ self-rated abilities to perform specific ablation procedures & satisfaction with training in surgical ablation for AF (y-axis numeric Likert values 1-5 correlate with survey response choices appearing in the methods section).
Our survey of senior CT surgery residents aimed to examine the training environment of surgical ablation for AF by evaluating various components of the resident experience though operative volume, case diversity, and clinical scenarios based on current guidelines. With the current recommendations and increasing prevalence of AF alongside safe and durable surgical techniques, it is likely that cardiac surgeons will be tasked with performing more ablations.[1-3] Given that incomplete ablation procedures have been demonstrated to yield worse long-term outcomes as compared to bi-atrial lesion sets with regard to maintenance of sinus rhythm it is imperative that graduating trainees are competent with both the indications for and performance of AF ablation surgery.[6]
Although this survey had a modest response rate, it is within expected response percentages for internet-based, non-incentivized, voluntary surveys with a single request for participation.[7] We acknowledge the potential for sampling error as the responders may not fully represent the entire cohort of senior CT surgery residents and may demonstrate bias toward dissatisfaction in training with ablation surgery. Indeed, those with more robust experiences may have elected not to respond. Nevertheless, while there may be training programs which have a much more robust experience in ablation surgery those programs are likely outliers rather than the norm across residencies. Additionally, it is unknown whether or not the contact information available from the TSDA contains email addresses that were functional or accessed by their owners during the survey administration. Regardless, there are important concerns identified from our results including the array of often-incomplete lesion sets (PVI), low case volume during residency, and inappropriate scenarios (aortic dissection, arrhythmia prophylaxis) or missed opportunities to perform an ablation. These findings would suggest a not-irrelevant proportion of residents being inadequately exposed to surgical ablation of AF. Although this survey focused on surgical ablation of AF, there may be other components of CT surgery residency training where residents are dissatisfied (for example: coronary artery bypass, aortic valve replacement). A comparison of perceptions of the training experience in various procedures may be of interest but is out of the scope of this work.
Current CT surgery residency graduation requirements mandate a minimum of 5 ablation surgeries of any type (PVI, bi-atrial, left atrial, etc.), which interestingly, matches our reported median case volume. With regard to training in other cardiac surgeries, minimum case volumes have been reported to demonstrate competency however these do not exist for surgical ablation. Yount and colleagues evaluated resident performance in coronary artery bypass surgery and identified 30 cases as being a level of significant improvement in operative conduct.[8] It is unknown whether or not the mandated 5 cases is sufficient; however, there is an appreciable range of skill required to perform a pulmonary vein isolation compared to a bi-atrial lesion set. Regardless, the likely inadequacy of the reported case volume is underscored by the respondents’ overall self-perceived inability to independently perform standardized full lesion sets and neutral satisfaction in their training. Whether or not the survey participants overestimated or undervalued their skills is unknown as is their case logging habits. Resident case volume reporting is subject to variation as prior reports have suggested residents may consider themselves the primary surgeon if they are merely present at the operation.[9] Thus there is a possibility that the actual number of ablation surgeries predominantly performed by a trainee is less than reported in our findings. Additionally, the survey may have captured residents with an additional 1-2 years of training remaining so those responders may graduate with a greater case volume.
Multiple opportunities exist for the improvement in training residents to perform surgical ablation for AF. While many leaders in the field of arrhythmia surgery provide seminars at professional meetings and industry-sponsored courses are available, formal and earlier exposure during residency has potential to strengthen a new/younger surgeon’s repertoire. As exposure to complete ablations and familiarization with the anatomic boundaries may be accomplished during residency training in the way of simulation, tissue labs or higher-fidelity models would likely be necessary alongside a complete curriculum and proficient instructors. However, increasing case volume would likely provide a more robust grasp of the nuances and sequence of the operation. Regardless, increasing case number hinges on the adequacy of the instruction by teaching surgeons, as educators must employ complete lesion sets.
The lack of exposure to complete ablations is again suggested by our findings of PVI being the most commonly employed lesion set. While likely sufficient for paroxysmal AF, PVI has been demonstrated to be inferior to complete bi-atrial lesions regarding long-term maintenance of sinus rhythm for persistent or longstanding persistent AF.[6] The Society of Thoracic Surgeons (STS) guidelines offer Class I recommendations for performing surgical ablation for AF at the time of mitral valve, aortic valve, coronary artery bypass, and combined valvular and coronary bypass operations. Additionally, surgical ablation for AF for symptomatic patients refractory to antiarrhythmic medications or catheter-based therapy is recommended at the IIa level. Finally, a bi-atrial lesion set is recommended over a PVI.[1] Despite the majority (77-98%) of responders’ adherence to the clinical scenarios in our survey based on the abovementioned guidelines, it is unknown if the residents would actually perform an ablation or complete lesion set in real time circumstances as well as if such recommendations are applied at their training program.
Possible barriers to adequate teaching by instructors include the perceptions that ablations risk increased morbidity and mortality, are time consuming, or yield no benefit to the patient. Despite data to the contrary, a persistently low percentage of surgeons perform ablations in appropriate settings.[5] Again, any improper training or technique of the supervising/instructing surgeon must be remedied so as to provide residents an appropriate exposure.
Conflicts/declarations of interest
none
Overall, our findings of incomplete lesion sets, low case volume, and neutral satisfaction with training should inform educators of the need to intervene on these issues or perform further evaluation. The importance of more thorough clinical instruction in surgical ablation for AF during CT surgery residency as well as the development of standardized curricula may yield improved patient outcomes and greater application of surgical ablation.