Safe Delivery of Endoscopic Brachytherapy in a Patient with a Dual Chamber Pacemaker
Chang Nancy Wang1, Cynthia Yeung1, Andres Enriquez1, Adrian Baranchuk 1
1
Division of Cardiology, Kingston Health Sciences Centre, Queen’s University, Kingston, Ontario, Canada.
In patients with advanced esophageal cancer, management of dysphagia is a challenge with significant implications on patient quality of life. Brachytherapy has been shown to be an effective and safe treatment option for symptoms related to dysphagia. The effect of endoscopic brachytherapy on patients with a cardiac implantable electronic device has not previously been described in literature.
We present an 89-year-old female with a dual chamber permanent pacemaker who elected to undergo palliative brachytherapy delivered via endoscopy for treatment of dysphagia secondary to locally advanced esophageal adenocarcinoma.
Key Words : Brachytherapy, Cardiac Implantable Electronic Devices (CIED), Pacemaker (PM).
Correspondence to: Adrian Baranchuk,
Professor of Medicine
Cardiac Electrophysiology and Pacing
76 Stuart St
Kingston General Hospital K7L 2V7
Queen's University
Esophageal cancer is the seventh most common cancer worldwide [1], and more than half of diagnosed patients are not surgical candidates either due to significant comorbidities or advanced cancer staging [2]. In these patients, dysphagia is a common presenting symptom associated with malnutrition, dehydration, renal failure, and increased risk of infection [3]. Intra-luminal brachytherapy is emerging as an increasingly popular treatment option due to its low complication rate, positive impact on health-related quality of life, and sustained effect on dysphagia palliation [4,5].
The effects of radiation delivered by brachytherapy on cardiac implantable electronic devices (CIEDs) are unknown. We describe a patient with a dual chamber pacemaker who received intra-luminal brachytherapy.
An 89-year-old female with a dual chamber permanent pacemaker (St. Jude Medical 2272 Assurity, St. Jude Medical 2088TC Tendril STS leads programmed in bipolar configuration) implanted due to symptomatic tachycardia-bradycardia syndrome presented with progressive dysphagia and weight loss. On endoscopy, she was found to have a circumferential distal esophageal adenocarcinoma spanning 6 cm in length. Staging CT scan showed mild adjacent lymphadenopathy with no evidence of metastatic disease. Given her advanced age and multiple comorbidities including atrial flutter/fibrillation and diastolic heart failure, she was deemed not to be a candidate for curative surgical resection. She did not wish to have chemotherapy, and opted for palliative brachytherapy for her significant dysphagia. She was non-dependent on her pacemaker. Device programming parameters are outlined in [Table 1].
Table 1. Dual chamber pacemaker programmed parameters.
| Mode |
DDDR |
| Lower Rate |
60 bpm |
| Higher Rate |
130 bpm |
| Sensed AV delay |
225 ms |
| Paced AV delay |
250 ms |
| Capture duration |
|
| Atrial |
0.4 ms |
| Ventricular |
0.4 ms |
| Percent pacing |
|
| Right atrial |
14 % |
| Ventricular |
5.3 % |
Abbreviations: bpm = beats per minute, ms = milliseconds
She underwent brachytherapy delivered via endoscopy over the course of two weeks, for a total of 1800 cGy over three treatment fractions with iridium-192. The distance from the first dwell position to the device was estimated to be 14 cm. On day 1 of treatment, metal oxide semiconductor field effect transistors (MOSFET) were applied to the area of the pacemaker and measured a daily dose of 6.1 cGy at the center of the device, and 7.5 cGy at the device edge closest to brachytherapy [Figure 1]. The estimated total cumulative dose was 18.27 cGy at the center of the device and 22.5 cGy at the nearest device edge, or 1.0% of the treatment dose. Device interrogation was performed before the first treatment and after the last treatment, which demonstrated no evidence of device malfunction. Pacing/sensing thresholds, lead impedance and battery life expectancy before and after brachytherapy are outlined in [Table 2]. No over-sensed events were found, and the patient remained asymptomatic throughout treatment with no signs of syncope, presyncope, palpitations or chest pain. The patient had excellent response at the one-month follow-up post-treatment, with complete resolution of her dysphagia.
Figure 1. A. Endoscopic brachytherapy in a patient with a pacemaker. B. Insertion of endoscope to the esophageal tumour burden. C. Aligning brachytherapy seeds with radiation treatment area. Green * = markers for distal and proximal limits of radiation treatment area in esophagus. Yellow arrows = brachytherapy seeds.
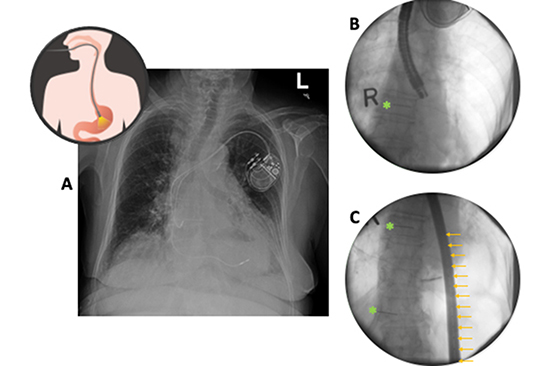
Table 2. Device interrogation parameters before and after brachytherapy.
|
Before Brachytherapy |
After Brachytherapy |
| Sensing amplitude |
|
|
| Atrial |
1.3 mV |
2.7 mV |
| Ventricular |
6.8 mV |
10.3 mV |
| Pacing Threshold |
|
|
| Atrial |
0.75 V |
0.5 V |
| Ventricular |
1.0 V |
0.75 V |
| Lead impedance |
|
|
| Atrial |
362 Ω |
350 Ω |
| Ventricular |
487 Ω |
362 Ω |
| Remaining longevity |
9.2-10.3 years |
8.5-9.3 years |
Abbreviations: V = volts, mV = millivolts, Ω = ohms
We have described the safe usage of palliative intra-luminal brachytherapy for the treatment of dysphagia in a patient with a dual chamber permanent pacemaker, with no evidence of device malfunction. We estimate that the patient’s device received a total cumulative dose of less than 25 cGy. In those who are pacing independent, a total cumulative radiation dose of less than 2 Gy is low risk for pacemaker dysfunction [6].
Brachytherapy remains an underutilized resource, perhaps due to limited availability of expertise. As there is growing awareness of esophageal stent-related complications in recent years[7], brachytherapy may be an increasingly popular alternative for management of dysphagia in esophageal cancer.
Similarly affected by the aging population, CIEDs are increasingly indicated in elderly patients [8]. Potential device malfunctions secondary to radiotherapy include over and under sensing, failure to capture, device mode reset, memory loss, battery depletion or complete device failure [9]. In comparison to direct external beam radiation, the effects of brachytherapy on devices are largely secondary to scatter radiation and electromagnetic interference. It is thought that scatter photon particles may cause excess electron-hole pairs in the silicon dioxide insulator causing accumulation of a net positive charge. The effect of scatter radiation on CIEDs is unclear, though small radiation doses (>2 Gy) are unlikely to result in predictable malfunction [10]. While the incidence of CIED complications due to radiotherapy is low, the rising population of patients with CIEDs requiring radiotherapy brings to attention the need for universal, evidence-based guidelines for the management of such patients[6]. A structured multidisciplinary approach involving collaboration between radiation oncology and cardiology is essential to minimize the incidence of device malfunction [11].
Palliative brachytherapy is likely safe for the management of dysphagia secondary to esophageal cancer in patients with CIEDs. However, further studies are required to better characterize the effect of brachytherapy on such devices.