Atrium-Atrioventricular Node Conduction Block
during Catheter Ablation of Persistent Atrial
Fibrillation
Yoshihide Takahashi, MD
The Cardiovascular Center, Yokosuka Kyousai Hospital, Yokosuka, Japan..
Previous studies have suggested that fibrillatory substrates are widely distributed in both atria in patients with persistent atrial fibrillation. Extensive bi-atrial ablation has been increasingly performed to improve the clinical outcomes; however, this may adversely affect the intra-atrial conduction during sinus rhythm. The worst con- sequence of an intra-atrial conduction disturbance is conduction block between the atrium and atrioventricular node. There have been a few case reports on this complication, which suggest that the conduction block may occur more. This review aimed to describe the risk factors and method of prevention of atrium-atrioventric-ular node conduction block.
Correspondence to: Yoshihide Takahashi, MD, Cardiovascular Center, Yokosuka Kyousai Hospital, Yonegahama-dori
1-16, Yokosuka, Kanagawa, Japan, 238-8558.
Catheter ablation of atrial fibrillation (AF) was ini tially performed in patients with paroxysmal AF. With the development of various technologies, pulmonary vein (PV) isolation has been applied also in patients with persistent AF. However, the clinical outcome of PV isolation in persistent AF has been limited as compared to paroxysmal AF.
To improve the efficacy of the catheter ablation of persistent AF, ablation techniques to modify the atrial substrate have been developed in the last decade. Currently, linear ablation and abla- tion targeting complex fractionated atrial elec- trograms (CFAE) are commonly performed to modify the atrial substrate, in which the atrial tissue in the left atrium (LA) is dominantly tar- geted but occasionally the right atrium (RA) also.
One of the possible mechanisms of such an ex- tensive ablation for maintenance of sinus rhythm is compartmentalization of the atria, which may interrupt the propagation of fibrillatory wave- fronts and terminate AF. However, the ab- lation lesions may also interrupt the normal intra-atrial conduction during sinus rhythm.
Atrium-atrioventricular (AV) node conduction block is one of the complications particularly associated with catheter ablation in the RA. This complication has been reported rarely, but may occur more often with the increased use of RA substrate modification. The aim of this review article was to discuss the ablation techniques potentially associ- ated with atrium-AV node conduction block and the method of prevention of this complication.
Efficacy of Right Atrial Substrate Mod-
ification
Atrium-AV node conduction block cannot occur unless ablation is performed in the RA, because the pathways from the sinus node to the AV node cannot be affected by ablation of the LA tissue alone. Arrhythmogenic substrates are more like- ly to develop in the LA, including the PV region, rather than the RA. Thus, ablation is usually be- gun with PV isolation, and then substrate modi- fication is performed in the LA if necessary. The efficacy of RA ablation is controversial. One ran- domized study demonstrated that the efficacy of bi-atrial ablation was similar to that of LA ablation;1 however some investigators consider that RA ablation is effective in selected patients.2-4 In a previous study, LA ablation was performed in the first procedure in patients with persistent AF.2 In the patients with recurrences of AF after the first ablation, a repeat ablation was performed, in which the RA was targeted. As a result, the RA ablation eliminated the AF in 62% of the patients who presented with AF after the first procedure.
The predictor of a requirement for RA ablation was the duration of persistent AF. The best cut- off for the duration of persistent AF for predicting the elimination of AF by ablation of the LA alone was 1.9 years. The results of this study suggested that patients with greater duration of continuous AF may benefit from RA ablation in combination with PV isolation and LA substrate modification.
A gradient in the AF cycle length between the LA and RA during catheter ablation suggests the re- quirement of RA ablation. According to the moth- er rotor theory proposed by Jalife et al.5 short cycle length activity is considered to drive the atria. Thus, short cycle length activity is the crucial site for maintaining AF, thereby being an optimal target for AF ablation. Hocini et al. reported that PV isolation and LA substrate modification increased the AF cy- cle length in the LA but failed to increase that in the RA in 19% of patients with persistent AF, and addi- tional RA ablation was effective in those patients.3 From the results of these studies, the RA needs to be considered as a target for ablation in patients in whom LA ablation failed to maintain sinus rhythm.
Lesion Set in the Right Atrium
As mentioned above, particularly in patients with longstanding persistent AF, AF substrates may exist also in the RA. There has been no pre-determined lesion set in the RA which has shown some efficacy. Ablation of a particular site can terminate AF in an individual patient, suggesting the driving role of the site. In most of other patients, however, ablation of that site fails to affect fibrillatory process. It is there- fore considered that the AF substrate is not localized to some specific anatomical structures in the RA.
RA substrate modification is usually guided by the local atrial electrograms, such as continuous activity.6 In the posterior RA, CFAE is commonly dis- played. When radiofrequency (RF) energy is de- livered in the posterior wall of the RA, an ablation catheter is dragged from the superior vena cava to the inferior vena cava. This ablation lesion is often called as an “intercaval line”. Organization of the local atrial activity is an optimal endpoint. Howev- er, this ablation technique may inadvertently result in conduction disturbances between the RA lateral wall and interatrial septum. Additionally, cavo-tri- cuspid isthmus (CTI) line is frequently ablated for the prevention of macro-reentry around the tricus- pid annulus in patients with persistent AF. If the intercaval line and CTI line become blocked, the anterior wall of the RA will be the sole pathway of the activation wavefront from the sinus node to the AV node. CTI ablation may alter slow pathway of the AV node also.7 After catheter ablation in the posterior wall of the RA and CTI, a conduction dis- turbance in the anterior wall or antero-septum of the RA or injury of fast pathway can result in conduction block between the atrium and AV node
Complete conduction block in the normal atrial tissue is often infeasible, because of the require- ment for a considerable amount of RF energy to be delivered. However, we can readily achieve com- plete conduction block in the injured atrial tissue, such as with spontaneous scarring or iatrogenic scarring associated with previous cardiac surgery or previously ablated lesions. Patients who have undergone previous ablation or cardiac surgery are at increased risk of conduction block between the atrium and AV node during catheter ablation. It is important to know the prior lesion set before the catheter ablation for the prevention of this com- plication. Administration of antiarrhythmics may exacerbate intra-atrial conduction disturbances.
There have been some reports of atrium-AV node conduction block occurring during catheter abla- tion of persistent AF. One was a case of a patient who had myocarditis and previously underwent Maze procedure.8 RF delivery from the lateral wall to the posterior wall of the RA resulted in atrium-AV node conduction block. Presumably, this patient had had conduction block along the intercaval line and anterior wall of the RA. This conduction block may have been due to the lesions deployed in the prior Maze procedure and possibly also have been due to spontaneous scarring from myocarditis.
In another report, atrium-AV node conduction block occurred during CTI ablation in a repeat pro- cedure.9 This patient had previously undergone extensive ablation, particularly in the interatrial septum. The prior RF lesions in the interatrial sep- tum might have blocked the connection between the interatrial septum and AV node or fast path- way of the AV node. Then, CTI ablation blocked the last connection between the RA and AV node or slow pathway. In both cases, pacemaker was not implanted. Former patient had recurrence of AF 3 weeks after the procedure, and latter patient was in junctional rhythm with heart rate of 50 bpm.
Prevention of Atrium-Atrioventricular Node Conduction Block
To identify risk factors is useful for the prevention of atrium-AV node conduction block. Prior cardiac surgery or extensive atrial ablation in the RA is a risk factor. In addition, patients with atrial myo-cardial disease such as myocarditis, or significantly enlarged RA are at risk. The prolonged PR interval or slow ventricular response during AF may suggest preexisting conduction distur- bances between the sinus node and AV node or within the AV node. In such patients, therefore, a voltage map using a 3D mapping system before catheter ablation would be helpful to identify intra-atrial conduction disturbances (Figure A and B). Low-voltage atrial tissue may represent the local conduction block or the presence of injured atrial tissue where RF delivery can block local conduction. Thus, care must be taken when RF is delivered in the low-voltage areas. If low-voltage areas are distributed extensively in the RA, sub- strate modification in the RA is not recommended.
Figure 1A Postero-lateral view of an activation map of the right atrium (RA) during sinus rhythm using CARTO system in a patient with prior cardiac surgery The blue dot represents the earliest activation site at the middle of the posterior RA.
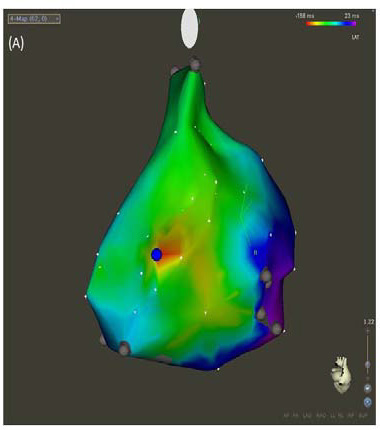
Figure 1B A bipolar voltage map of the RA during sinus rhythm in the same patient as shown in (Figure 1B). The purple represents areas with bipolar voltages of ≥0.5mV. Low-voltage areas (< 0.5mV) were present in the posterior and lateral wall of the RA including the sinus node. A linear lesion connecting two low-voltage areas (red lines) may result in atrium-AV node conduction block.
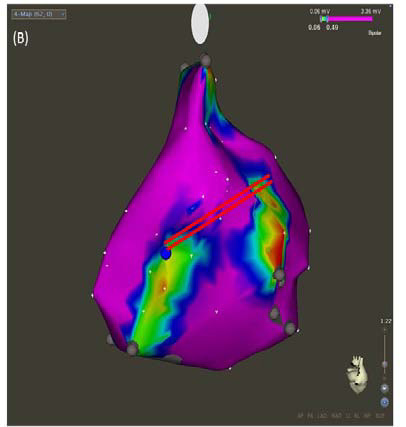
The development of ablation techniques and tech- nologies has enabled us to maintain sinus rhythm even in patients with extensive atrial substrates. Successful catheter ablation in such patients re- quires extensive bi-atrial ablation, which may ad- versely result in conduction block between the atri- um and AV node after restoration of sinus rhythm. The preexisting spontaneous or iatrogenic scarring, which can be evaluated by a 3D voltage map, is asso- ciated with such a complication. The evaluation of the PR interval during sinus rhythm or ventricular rate during AF is also useful for estimating the risk