Risk of Arrhythmia Recurrence After Successful Ablation of Lone Atrial Fibrillation
Khaykin Y, MD, Friedlander D, BSc, Zarnett L, BSc, Seabrook C,RN, Beardsall M, RN, Feltham S, RN, Tsang B, MD, Wulffhart Z, MD, Pantano A, MD, Verma A, MD.
Department of medicine, university of toronto
.
Correspondence to: Yaariv Khaykin Address: 105-712 Davis Drive, Newmarket, Ontario, L4E 4M5.
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia and is difficult to treat.1 It may present with a variety of symptoms ranging in severity from mild to disabling.2 While some patients get diagnosed at the time of a routine visit and are not aware of their arrhythmia, others may present with palpitations, chest discomfort, dyspnea and syncope. Atrial fibrillation is commonly associated with cardiac and extra cardiac conditions such as valve disease, left ventricular dysfunction, hypertension, diabetes, pulmonary and thyroid disease.3
Patients with AF and structural heart disease or hypertension are at a particularly high risk of developing significant functional impairment or frank congestive heart failure.4 This is related to diastolic dysfunction whereby patients depend heavily on the atrial ‘kick’ and a controlled regular heart rate for ventricular filling. If these conditions are not met, the filling pressure briskly rises leading to pulmonary congestion.
As part of an adaptation response, left atrium may dilate to be able to accommodate a larger volume of blood, compensate for lack of atrial contraction, and moderate the increase in pulmonary pressures. In turn, left atrial enlargement may signify increased atrial scarring and promote atrial fibrillation by providing a suitable electromechanical substrate for reentry.5
Unfortunately, AF is not unique to patients with other comorbidities. Patients without any discernable heart disease or systemic conditions may have so called ‘lone’ atrial fibrillation accounting for about 3% of patients with AF.6 The definition of lone atrial fibrillation varies between publications and typically excludes patients with AF and significant structural heart disease defined as left ventricular ejection fraction less than 40%, moderate or severe aortic or mitral valvular insufficiency or stenosis, or history of prior heart surgery. According to the guideline definition, patients with thromboembolic risk factors of hypertension, diabetes or prior stroke should be excluded along with patients suffering from congestive heart failure, significant pulmonary or thyroid disease.7 Given accumulating body of evidence linking obstructive sleep apnea (OSA) and atrial fibrillation, patients suffering from OSA should be excluded.8 Finally, given known association between AF and left atrial enlargement, those with left atrial size greater than normal may be qualified as having plausible etiology for their arrhythmia. It is certainly plausible that myocardial fibrosis in the left atrium and left atrial dilatation may also be the result rather than the cause of AF in some patients. At the same time, based on the purported explanations for the maintenance of AF which include multiple wavelet reentry, it is known, thatgreater myocardial mass and larger atria form better substrate for re-entry.9 Atrial fibrillationmay be more prevalent in taller people who also happen to have larger atria.10-13 While that does not mean that the relationship of larger atria and atrial fibrillation is always causative, it certainly suggests that it is true in many instances and as such may form the basis for AF in these patients. While determining left atrial volume index may be the preferred method for identifying such patients, this measurement is frequently lacking in clinical practice leaving the clinicians with left atrial diameter, typically measured during transthoracic echocardiography procedures in the long parasternal axis.
Atrial fibrillation is present in as many as 10% of the octagenarians.6,11,14 Advanced age among patients with AF (greater than 65-75 years of age) is an independent risk factor for embolic events. Accordingly, patients over 75 are not typically classified as having lone arrhythmia.7
Our options for managing atrial fibrillation have improved tremendously over the years. Domains of care for these patients include treatment of co-existent conditions, prevention of thromboembolic events, medical or interventional control of the ventricular response rate and symptom relief, which typically involves conversion to sinus rhythm and its long-term maintenance.
The latter can be achieved medically in some patients using antiarrhythmic medications. Unfortunately, all of these are fraught with side effects, frequently outweighing the benefits of their use, and are not very effective. The best yet most toxic antiarrhythmic drug, amiodarone, provides rhythm control up to 60% of the time at best.15
Discovery of the pulmonary vein ectopic events initiating atrial fibrillation has lead to a revolution in AF management, whereby ablative therapy initially aimed at elimination of the sources of ectopic activity, ostial isolation of the pulmonary veins and, more recently, isolation of the pulmonary vein antra, can now be offered to patients suffering from AF who cannot or prefer not to take antiarrhythmic medication.16-18
Ablation is particularly important to consider as an option in patients with lone atrial fibrillation. These patients are typically at low risk of an embolicevent, do not have other comorbidities requiring management, and are frequently young, anxious and highly symptomatic for palpitations and functional impairment as a result of their arrhythmia. While some prefer antiarrhythmic drug therapy, when given the opportunity, most of these patients choose ablation, stating unwillingness to be on long-term medication or medication side effects, particularly lack of energy related to the use of most drugs in this class.
There is little published literature addressing outcomes of catheter ablation in patients with lone atrial fibrillation. Most of the literature addresses surgical therapy in these patients. Patients with lone AF in the surgical literature are typically defined as those who do not require any other surgical intervention beyond a modified Maze procedure for their arrhythmia. While there is some overlap between these patients and patients undergoing catheter ablation, few young and otherwise healthy patients choose to undergo surgical therapy for their arrhythmia as a stand-alone procedure and many patients thus treated are older and have other comorbidities. Discussion of surgical AF therapy for lone AF is outside of the scope of this review.
Rather than examine outcomes among patients with lone AF vs others, most of the literature on catheter ablation divides patients into those with paroxysmal or non-paroxysmal arrhythmia, and further stratifies patients by age and other comorbid conditions. We identified only three prior publications focusing specifically on the outcomes of catheter ablation in patients with lone atrial fibrillation. All arrhythmia recurrences are defined as any episode of atrial fibrillation of at least 30 seconds in duration.19
In the first paper, Khaykin et al. defined lone AF patients based on absence of left ventricular dysfunction (ejection fraction < 40%), moderate or worse aortic or mitral valvular insufficiency or stenosis, or prior history of heart surgery.20 This is the largest reported cohort of patients with lone atrial fibrillation undergoing ablation at 194 patients. Lone AF patients in this study were young (54±12 years), but had relatively large left atria at 44±24 mm in diameter; 3.5% of the patients were in NYHA II-III functional class. They had prevideously failed 3.2±1.1 antiarrhythmic drugs. Only 58% of these patients had paroxysmal AF. Patients in this study underwent pulmonary vein antrum isolation (PVAI) guided by a circular mapping catheter. Intracardiac echocardiography was used during the majority of procedures.
The authors presented long-term follow-up of 18±7 months. During that time 16% had a late recurrence beyond the three-month blanking period, 2% were controlled on antiarrhythmic drugs and 14% of the patients had repeat procedures. The rate of significant complications was 4.1%, in line with that reported in other contemporary studies.
In a series of patients undergoing AF ablation reported by Calvo et al.,21 107 patients had lone AF, defined as arrhythmia in patients under 60 years of age and without hypertension, thyroid disease, clinical or echocardiographic evidence of cardiopulmonary disease. Left atrial size in these patients was normal at 39±6 mm. Paroxysmal AF was present in 74% of the patients studied.
Patients in this study underwent circumferential pulmonary vein ablation (CPVA) using the CARTO (Biosense Webster, Diamond Bar, CA) 3D mapping system and incorporating a left atrial roof line, posterior line and a mitral isthmus line in the lesion set. Isolation of the posterior left atrium but not block across the mitral isthmus line was verified by the operators.
One year following the procedure, 59% of the patients with lone AF were free of recurrent arrhythmia. The rate of complications among these patients was similar to the study reported byKhaykin et al. at 4.3%.
Another study evaluated first-line cryoballoon ablation with pulmonary vein isolation verified using a circular mapping catheter and insured with focal radiofrequency ablation as necessary in 18 patients with paroxysmal lone AF defined as AF in the absence of structural heart disease.22 One of the patients had diabetes; left atrial size was normal at 39±4 mm among study patients. After a mean follow-up of 14±9 months, 89% of the patients were free from recurrent AF off antiarrhythmic drugs. One of the patients in this study developed transient phrenic palsy and another had to have surgical repair for a pseudoaneurysm at a vascular access site.
A study reported by De Potter et al.,23 compared outcomes of AF ablation in patients with and without reduced left ventricular ejection fraction (LVEF). In this study, 56% of the 36 patients without depressed LVEF (defined as LVEF ≥ 50%) did not have recurrent AF after a median follow-up of 16±13 months following CPVA performed using the same approach as that reported by Calvo et al.
In all of these studies, the likelihood of freedom from recurrent AF was similar among patients with and without lone atrial fibrillation.
Between February 2004 and May 2011, 458 patients with paroxysmal atrial fibrillation underwent PVAI guided by a circular mapping catheter and intracardiac echocardiography at our center. Details of the ablation procedure have been previously described.24 There does not appear to be a relevant influence of age on recurrences of atrial tachycardias after persistent AF ablation as indicated in different studies.17 -19
Having defined lone AF as AF in patients under 75 years of age, without structural heart disease, any of the CHADS-2 score components or left atrial enlargement beyond 40 mm, 60 of the ablation patients qualified as having lone AF (13%). table 1compares baseline characteristics of patients with lone AF vs others. Apart from the difference in factors defining lone AF, these patients had a lower BMI and have previously failed fewer antiarrhythmic drugs. Fewer lone AF patients failed amiodarone.
Table 1. Baseline Characteristics
| Parameter |
Lone PAF (n=60) |
Non-Lone PAF (n=398) |
p-value |
| Age |
47 ± 8.7 |
60 ± 9.9 |
<0.0001 |
| Male |
42 |
272 |
0.80 |
| BMI |
27 ± 4 |
29 ± 6 |
0.02 |
| AF duration (yrs) |
6.0 ± 5.1 |
7.4 ± 6.2 |
0.14 |
| #Failed AADs |
1.4 ± 0.9 |
1.7 ± 1.1 |
0.04 |
| Failed amiodarone |
11 (18) |
142 (36) |
0.008 |
| LA size (mm) |
36.8 ± 2.97 |
41.7 ± 4.93 |
<0.0001 |
| Hypertension |
|
218 (55) |
|
| Diabetes |
|
48 (12) |
|
| Structural Heart Disease |
|
166 (42) |
|
| Valve disease |
|
73 (18) |
|
| Significant coronary artery disease |
|
59 (15) |
|
| Cardiomyopathy1 |
|
34 (8) |
|
| History of Prior Heart Surgery |
|
16 (4) |
|
Data are expressed as mean ± SD or number (%) of patients.1Left Ventricular Ejection Fraction less than 40%, clinical diagnosis of hypertrophic or dilated cardiomyopathy
As seen in table 2, procedural characteristics were similar between the two groups of patients. Following ablation, however, patients with lone atrial fibrillation were far less likely to be treated with statins or ACE inhibitors as would be expected based on their selection criteria. Patients with lone AF were followed for 1.8±1.5 years on average compared to 2.0±1.6 years for the other patients (p=0.3). Eighteen patients (30%) with lone AF had an early recurrence during the 3 month blanking period following the procedure compared to 173 (43%, p=0.05 vs lone AF) patients with non-lone AF. Twenty-six patients with lone AF (43%) had a late recurrence beyond the blanking period vs 195 (50%, p=0.34) patients with non-lone AF. There was a trend to longer time to late recurrence among patients with lone AF with a mean time to late recurrence of 13±16 months vs 10±10 months in the other group (p=0.1). The difference in the rate of AF recurrence over time reached statistical significance in Kaplan-Meier analysis (p<0.05,figure 1) with curves representing survival free of recurrent arrhythmia separating after 6 months of follow-up. Patients with lone AF were just as likely to have repeat ablation procedures following the initial procedure as illustrated in table 2.
Figure 1. Survival Free of Atrial Fibrillation
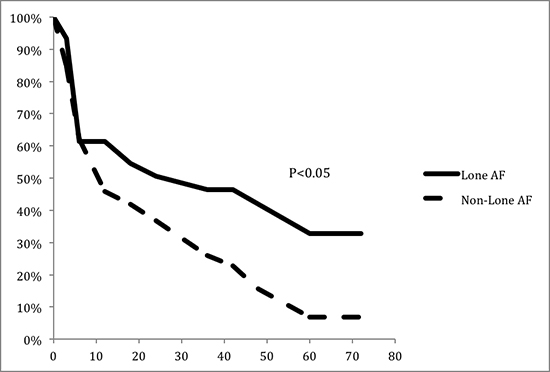
Time following ablation, months
Table 2. Procedural Details
| Parameter |
Lone PAF (n=60) |
non-Lone PAF (n=398) |
p-value |
| Irrigated catheter |
28 (47) |
145 (36) |
0.13 |
| Concurrent atrial flutter ablation |
5 (8) |
55 (14) |
0.24 |
| Fluoroscopy time (min) |
73 ± 28 |
74 ± 24 |
0.87 |
| Procedure time (min) |
206 ± 61 |
212 ± 89 |
0.63 |
| RF time (min) |
89 ± 34 |
89 ± 38 |
0.93 |
| Statins post ablation |
8 (13) |
167 (42) |
<0.0001 |
| ACEi post ablation |
2 (3) |
113 (28) |
<0.0001 |
Data are expressed as mean ± SD or number (%) of patients
Table 3. Repeat Ablation Procedures
| Parameter |
Lone PAF (n=60) |
non-Lone PAF (n=398) |
p-value |
| Number of Procedures |
|
|
|
| 1 |
40 (67) |
272 (68) |
0.80 |
| 2 |
17 (28) |
102 (26) |
0.66 |
| 3 |
3 (5) |
22 (6) |
0.87 |
| 4 |
0 (0) |
2 (0.5) |
0.58 |
Data are expressed as number (%) of patients
The definition of lone atrial fibrillation in the literature is inconsistent between studies. Based on the guidelines, lone AF should be defined as atrial fibrillation in patients under 75 years of age without structural heart disease, including left atrial enlargement and without any of the CHADS-2 risk factors for thromboembolic events. We believe thatthis definition should also exclude patients with history of heart surgery or any comorbidities known to be associated with AF, such as pulmonary and thyroid disorders as well as obstructive sleep apnea, based on available evidence. Patients with lone atrial fibrillation may present with either paroxysmal or persistent arrhythmia.
Prevalence of lone AF among patients presenting for ablation is significantly higher than what is reported in the medical literature. This may be expected since many lone AF patients would prefer ablative therapy to long-term medical management.
Surprisingly, regardless of the ablative approach used, outcomes in patients with lone atrial fibrillation are similar to those in patients who have risk factors for thromboembolism or other comorbid conditions known to associate with AF, although based on our data, time to recurrence of AF following ablation is longer among patients with lone paroxysmal AF compared to other paroxysmal AF patients, presumably secondary to a healthier left atrial substrate. One-year success rate of ablation among lone AF patients ranges from 56% to 89% depending on the study, definition of lone AF and approach used with little data on long-term follow-up in this group of patients.
Experience at our center suggests that lone AF patients do derive a greater long-term benefit compared to other patients presenting for AF ablation. At the same time cost effectiveness of ablation in this group of patients is suspect based on some published estimates25 and the rate of procedural complications, while similar to the general AF population, is excessive given their low baseline risk.
Further epidemiological studies are necessary to better define the prevalence of lone AF among patients treated with ablation as well as procedural cost effectiveness. These studies should also pay close attention to the risks of ablation in this otherwise low-risk group of patients.