Atrial fibrillation is expected to affect an estimated 12-15 million people in the United States by the year 2050.1,2 This increasing incidence and prevalence is greatest amongst the elderly (patients greater than 70 years of age), with nearly 8% of those older than 70 carrying a diagnosis of atrial fibrillation.3-6 Three out of four patients with atrial fibrillation are between the ages of 65 and 85.7,8 Age carries particular risk amongst patients with atrial fibrillation, as evidenced by the increased stroke risk in patients greater than 75 years of age.4,9-10 Management of atrial fibrillation in the elderly presents unique challenges, including issues related to bleeding, general debility, a greater incidence of underlying conduction system disease, and structural heart disease.
Decision making regarding the management of atrial fibrillation in the elderly includes issues related to anticoagulation and whether to focus on a rate versus rhythm control approach. Perhaps the most important question that needs to be answered in this patient population is whether they are symptomatic from atrial fibrillation as this may be the most important factor in favor of pursuing a rhythm control strategy. Symptomatology from atrial fibrillation itself needs to be differentiated from symptoms due to a rapid ventricular response associated with atrial fibrillation as the latter would entail an aggressive rate control strategy, which may include atrioventricular junction ablation and pacemaker implantation, while the former would entail an approach geared more towards rhythm control. The risk of tachycardia-bradycardia syndrome and sick sinus syndrome may also be more common in elderly patients and favor a rhythm control approach as a more desirable option in many patients.11,12 The options for rhythm control include antiarrhythmic medications and pulmonary vein isolation. There is a lack of prospective data on the relative benefits of these different rhythm control strategies in the elderly population.13-16 Antiarrhythmic drugs can be difficult to manage due to unpredictable metabolism in elderly patients and intolerance of side effects.17 Thus, pulmonary vein isolation and ablation of non-pulmonary vein foci is an important alternative in the management of atrial fibrillation in the elderly.
Atrial fibrillation is thought to be triggered by foci of abnormal conduction that lead to fibrillatory conduction in the atria. One of the mechanisms underlying the pathogenesis of atrial fibrillation is thought to be atrial remodeling, whether due to chronic stress from factors such as high atrial pressures from diastolic or systolic failure or from loss of atrial muscle mass resulting in greater dispersion of atrial refractoriness.18-20 Multiple studies have shown a role for fibrosis in the pathogenesis of atrial fibrillation.19 In the elderly, multiple factors including diastolic dysfunction, hypertension, and age-related loss of muscle mass may lead to increased left atrial stretch and fibrosis with a greater predilection towards developing atrial fibrillation.16 Furthermore, sinus node dysfunction and reduction of normal conduction velocities throughout the atria may occur more commonly in elderly patients, resulting in a greater likelihood for secondary foci to take control and degenerate into atrial fibrillation.
The importance of recognition of atrial fibrillation in the elderly lies in both its association with increased risk of morbidity and mortality, and in its leading to significant healthcare costs related to recurrent hospitalizations and doctor’s visits for the primary arrhythmia and its secondary effects.21,22 Atrial fibrillation has been associated with an increased risk of stroke, heart failure, and overall mortality, particularly in elderly patients. 2,22 Furthermore, due to the risk of stroke, employment of anticoagulation strategies may increase bleeding risk, which may be higher in elderly patients above the age of 80, and is also associated with the need for frequent monitoring.23-25 Patients may present with symptoms related to rapid rates but also with heart failure exacerbation, stroke, or bleeding from concomitant anticoagulation use. Thus, close management of atrial fibrillation is necessary, but may also prove a significant challenge.
Several ablation strategies exist for the treatment of atrial fibrillation, but may be separated grossly into rate control via atrioventricular junction ablation or rhythm control via ablation of focal triggers of atrial fibrillation.26 The latter strategy involves isolation of the pulmonary veins by creating effective areas of electrophysiological silence surrounding the ostia of the pulmonary veins, thereby eliminating transmission of signals from these venous foci.26 However, several non-pulmonary vein foci may also exist and may necessitate additional ablation at other sites. Atrioventricular junction ablation is definitive in its control of patients’ rates but results in 100% pacemaker dependence. This may cause issues related to the long-term need for pacemaker follow-up and care, the risk of heart failure related to chronic right ventricular pacing, and the limitations in rate-responsiveness algorithms that may not always offer the level of heart rate augmentation to a given set of external stimuli that would be seen in a natural state. Studies have suggested, however, that atrioventricular junction ablation to achieve rate control is both a safe and well tolerated option in many patients.27-29 Atrioventricular junction ablation may be a reasonable option in elderly patients in whom rate control cannot be achieved with medical therapy and in whom the duration of chronic right ventricular pacing may not be sufficient enough to cause significant cardiomyopathy.
In contrast, pulmonary vein isolation focuses on maintenance of sinus rhythm. While effective in up to 70% of all-comers with paroxysmal atrial fibrillation, the efficacy of this strategy in an elderly cohort has not been as well established.30,31 Ablation aimed at maintenance of sinus rhythm may offer the benefit of maintaining atrio-ventricular synchrony while simultaneously limiting the need for potentially caustic antiarrhythmic or rate control agents that may often be poorly tolerated in elderly patients. Furthermore, in the absence of underlying sinus or atrioventricular nodal disease, patients will generally not need additional device therapy that may lead to additional long-term risks. However, many patients may require multiple ablation attempts to achieve long-term maintenance of sinus rhythm.26
Efficacy of Pulmonary Vein Isolation in the Elderly
As mentioned previously, the first step in the management of atrial fibrillation in the elderly is deciding whether a rate or rhythm control strategy is appropriate. While prior trials have suggested that rate and rhythm control strategies have equivalent survival, post hoc analyses have suggested that successful maintenance of sinus rhythm was an independent predictor of improved survival. Furthermore, comparison between rate and rhythm control strategies have always involved use of antiarrhythmic drugs, which often have poor side effect profiles and may be proarrhythmic in some patients. There are no published prospective trials to date comparing ablation-based rhythm control against a rate control strategy. However, it is clear that restoring and maintaining sinus rhythm in certain patients may confer both a morbidity and mortality benefit.33 Thus, the decision to employ pulmonary vein isolation or trigger-focused ablation as a management strategy in elderly patients needs to take into account the goals of rhythm control and whether it may be as efficacious as in younger patients who comprise most of the cohorts studied to date.
Table 1. Baseline Clinical Characteristics.
| Study |
Number |
Quinidine |
Propafenone |
|
p-value |
| Bhargava, et al34 |
103 |
>60 |
82% (vs 85%) |
6.8% (vs 2.8%) |
AF Ablation in <50 years old |
| Hsieh, et al35 |
37 |
>65 |
81% (vs 100%)* |
0% (vs 0%) |
AV nodal ablation + pacemaker |
| Zado, et al36 |
32 |
>75 |
87% (vs 89%) |
2.9% (vs 1.6%) |
AF Ablation in <65 years old, |
| Corrado, et al37 |
174 |
>75 |
93% |
1.0% |
N/A |
| Nademanee, et al40 |
635 |
>65 |
81% |
3.1% |
N/A |
| Traub, et al15 |
15 |
>70 |
60% (vs 80%) |
6.7% (vs 4.4%) |
AF Ablation in <70 years old |
| Kusumoto, et al41 |
61 |
>75 |
82% (vs 96%) |
0% (vs 1.1%) |
AF Ablation in <65 years old |
| Bunch, et al42 |
35 |
>80 |
78% (vs 75%) |
5.7% (vs 3.1%) |
AF Ablation in <80 years old |
| Hsu, et al38 |
22 |
>65 |
68% (vs 75% vs 71%) |
9.1% (vs 2% vs 0%) |
AF Ablation in 45-65 years, <45 years |
| Oral, et al39 |
24 |
>70 |
80% |
12.5%* |
N/A |
LV-EF: left ventricular ejection fraction AF: atrial fibrillation, CAD: coronary artery disease, DCM: dilatative cardiomiopathy, VHD: Valvular Heart Disease
Several studies have recently studied the efficacy and safety of pulmonary vein isolation in elderly patients, one of which was a prospective, nonrandomized trial comparing atrioventricular nodal ablation with pulmonary vein isolation.15,34-40Table 1 summarizes the data on atrial fibrillation ablation in the elderly including published trials to date, patient characteristics, and outcomes. Four of these studies focused on the efficacy and safety of pulmonary vein isolation in different age groups and the remaining studies focused on the relative overall safety of ablation in elderly patients. All studies involved segmental or circumferential pulmonary vein isolation with the addition of ablation of non-pulmonary vein triggers or linear ablation in the left atrium in some studies. The overall success rate across all studies, which included use of anti-arrhythmic drugs, was 80% and not age-dependent.Table 1
One of the key points of all the studies is that, despite the presumption that there may be greater amounts of fibrosis and atrial remodeling in elderly patients that limit efficacy of pulmonary vein isolation, there was no significant difference in success rates when compared with younger patients. Table 1 However, most of these studies included patients with paroxysmal atrial fibrillation. One study did focus on patients presenting with permanent atrial fibrillation and did demonstrate an age-independent success rate of about 70%.38
One limitation of the available data is that all of the studies, with the exception of the study by
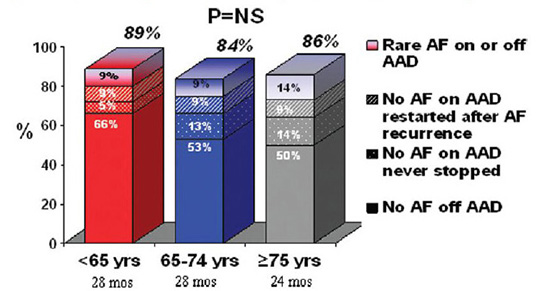
Corrado et al, have involved a single center with a high degree of experience. Also, decision making in retrospective analyses may be impacted by differences in choices related in how to achieve rhythm control. For example, in the study by Zado et al, patients over 75 years of age tended to undergo repeat ablation less often and more often remained on antiarrhythmic drugs than those less than 65 years of age despite similar overall success rates.(Figure 1) Continued use of antiarrhythmic medications was also seen in studies by Traub et al and Kusumoto et al.15,4 In the latter study, the similarity in the success of a rhythm control strategy in elderly patients compared to younger patients appeared due to the continued use of antiarrhythmic drugs rather than to the ablation strategy alone.
While no comparisons were made with younger age groups, the one multi-center study reported by Corrado et al showed similar efficacy in achieving sinus rhythm (82%) to that seen in the other single center trials.37 Thus, allowing for the limited numbers of patients included across trials and differences in techniques between trials, the efficacy of atrial fibrillation ablation in elderly patients appears to be similar to that of younger patients.
Safety of Pulmonary Vein Isolation in the Elderly
Another area of consideration when referring elderly patients for atrial fibrillation ablation is the safety of the procedure. Table 1 Elderly patients tend to have higher degrees of baseline stroke, hypertension, and structural heart disease than younger patients and thus, may be more prone to complications. One risk during pulmonary vein isolation is incidental cerebrovascular accident from coagulum formation and embolization during the procedure. Several older studies, including one multivariate analysis, have suggested that there are more major adverse clinical events in older patients, though these results have not necessarily borne out in more recent studies, which may be attributed to advances in catheter technology and more aggressive anticoagulation.15 Bunch et al, however, did demonstrate a longer duration of hospital stay in those over 80 year of age after ablation.The overall risk between studies of periprocedural cerebrovascular accident, cardiac tamponade or pulmonary vein stenosis ranged from 0 to 12% between studies.
One limitation in assessing safety of pulmonary vein isolation lies in the definition of cerebrovascular accident. Small incidental strokes may not be clinically evident, as is often seen in cardiac catheterization patients when delineating between clinically significant stroke with grossly apparent clinical features and silent cerebrovascular accidents that may be seen on direct imaging but otherwise not clinically apparent. The long-term risk of these issues in terms of cognitive functioning, however, is unclear and would require longer term follow-up of these patients. Preexisting cerebral atherosclerosis has been associated with increased risk of periprocedural major complications, though this may be attributed to a higher incidence of comorbidities such as hypertension, structural heart disease, and prior stroke with already diminished baseline functioning in these patients.32 Lastly, since all of the studies evaluating safety of ablation have been nonrandomized, the elderly patients who underwent ablation may have been a select population that is not representative of the general elderly population with atrial fibrillation.
Thus, the safety of pulmonary vein isolation, while not clearly different from younger patients, needs to be considered in the context of the limitations in existing studies and the presumed higher incidence of pre-existing conditions in elderly patients.
Atrioventricular Nodal Ablation Versus Pulmonary Vein Isolation
In certain patients, rate control of atrial fibrillation may be challenging and difficult to achieve with medications alone. Atrioventricular nodal ablation and pacemaker implantation may be used to achieve rate control in this population of patients. Several studies have demonstrated efficacy of this approach as being similar to that of antiarrhythmic drug use in terms of risk of sudden death or overall mortality. Furthermore, these patients tend to have survival rates similar to the general population.27-29
There has been one nonrandomized study directly comparing atrioventricular nodal ablation against pulmonary vein isolation in pharmacologically refractory elderly patients. While 100% of those patients with atrioventricular nodal ablation had control of their rates in atrial fibrillation, only 81% of those undergoing pulmonary vein isolation had rhythm or adequate rate control. However, 69% of patients undergoing atrioventricular nodal ablation still had persistent atrial fibrillation and 53% had congestive heart failure compared with 8% and 24% of patients undergoing pulmonary vein isolation respectively. In this study, patients undergoing atrioventricular nodal ablation and permanent pacing developed a higher incidence of heart failure, higher NYHA class, and a decreased left ventricular ejection fraction compared to the patients undergoing catheter ablation.
It is difficult to use the persistence of atrial fibrillation as an endpoint after atrioventricular nodal ablation given that this strategy involves primarily rate rather than rhythm control. However, the worsening of heart failure symptoms and decrease in ejection fraction are important considerations. There is some evidence that chronic right ventricular pacing may compromise cardiac function over time.However, another study that was not specific to elderly patients showed that atrioventricular nodal ablation plus biventricular pacemaker placement in patients with NYHA class II ablationto III symptoms tended to not see as great an improvement in heart failure symptoms as those who underwent pulmonary vein isolation (average age of patients = 60 + 8 years). Overall, these data suggest a rhythm control strategy in these patients may help overall functional status. However, the studies were nonrandomized, and programming of the pacemaker function was non-physiologic (all devices were programmed to VVI even in patients who later remained in sinus rhythm).
Thus, while several studies have demonstrated the safety and efficacy of atrioventricular nodal ablation with pacemaker implantation in managing ventricular rates and associated symptoms in atrial fibrillation, studies on effects on heart failure symptoms and further comparison with outcomes with pulmonary vein isolation are needed. It is still unclear if an atrioventricular nodal ablation approach is equivalent to a rhythm-control ablative strategy in terms of long-term morbidity and mortality.
Anticoagulation Management After Ablation
Conversion rate
The risk of stroke in atrial fibrillation is generally attributed to clot formation in the left atrium due to stagnation of blood in the left atrial appendage. Age greater than 75 years is one major component of the CHADS2 risk stratification used to determine the need for anticoagulation to reduce stroke risk atrial fibrillation. Elderly patients have a greater risk of stroke than younger patients with atrial fibrillation, but several studies have highlighted the greater bleeding risk with warfarin in this cohort.23,24 Two prior studies have suggested that if sinus rhythm is successfully maintained for up to 3-6 months after pulmonary vein isolation, anticoagulation may be discontinued.50 In the study by Corrado et al, warfarin was discontinued in 96% of elderly patients after atrial fibrillation ablation after 5-6 months in sinus rhythm without any incident strokes, despite a CHADS2 score > 2 in 65% of these patients. Current practices, however, tend to vary with regards to the decision to discontinue anticoagulation, especially given the risk.51 Ambulatory monitoring is often used to confirm sinus rhythm and the lack of recurrent, asymptomatic atrial fibrillation.13,40 Studies that have demonstrated the safety of this approach in determining the discontinuation of anticoagulation have involved small numbers of patients and have not been randomized. Thus, the safety of anticoagulation discontinuation after presumed successful pulmonary vein isolation, particularly in elderly patients who are often at greater risk of stroke, is unclear and at this time this decision must be left in the hands of the electrophysiologist performing the procedure after taking into account the individual risk profile of each patient.
Figure 1 Single center experience for patients completing at least 1 year of follow-up after ablationto
Several studies have suggested similar safety and efficacy of atrial fibrillation ablation in elderly patients when compared with younger patients. However, most of these studies have been single center trials with relatively small patient numbers. The potential benefits of achieving rhythm control in elderly patients relates to the maintenance of sinus rhythm, improvement in symptoms related to atrial fibrillation, and the potential for being able to discontinue anticoagulation. Several studies have demonstrated maintenance of sinus rhythm as a major determinant of improvement in outcomes and quality of life in patients with atrial fibrillation.33,52 Recent data also suggests the benefit in terms of quality of life and cost-effectiveness of pulmonary vein isolation over pharmacologic management strategies. Furthermore, given the potential for bleeding in Reviewelderly patients, the possibility that anticoagulation may be discontinued should be considered.
Atrioventricular nodal ablation and pacemaker implantation is another strategy that may be safe in select patients. However, close attention to the type of pacemaker (biventricular versus single versus dual chamber), the programming, and the patient’s functional status is likely needed to select those who will benefit most. Furthermore, there is limited data comparing the relative efficacy of this approach, in which patients may remain in atrial fibrillation but with better controlled ventricular rates, with that of pulmonary vein isolation trigger-guided ablation, in which maintenance of sinus rhythm is the principal goal.
To date, published data support that ablative strategies are relatively safe and efficacious in elderly patients. Future randomized prospective trials are needed to further assess the safety and efficacy of pulmonary vein isolation in elderly patients. Elderly subsets of the CABANA trial may offer some insights into the relative efficacy of pulmonary vein isolation when compared with antiarrhythmic drugs in managing patients with atrial fibrillation. Further studies are needed to better evaluate the relative benefits and risks of different approaches aimed at rate versus rhythm control in the elderly population and specifically, the role and timing of ablation strategies.