Reducing Ionizing Radiation Associated with Atrial Fibrillation Ablation:
An Ultrasound-Guided Approach
Nisha L. Bhatia, MD1, Arshad Jahangir, MD1, William Pavlicek, PhD2, Luis R.P. Scott, MD1, Gregory T. Altemose, MD1, Komandoor Srivathsan, MD1
1Division of Cardiovascular Diseases, Mayo Clinic College of Medicine, Scottsdale, AZ, USA.2Department of Radiology, Mayo Clinic College of Medicine, Scottsdale, AZ, USA.
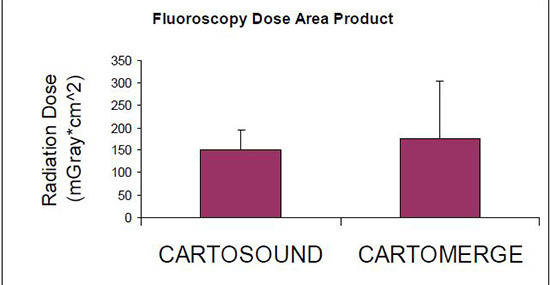
Radiation exposure with cardiac interventional procedures is an emerging concern. Patients receiving radiofrequency ablation for atrial fibrillation (AF) still routinely undergo pre-ablation computed tomography (CT) scans for definition of left atrial and pulmonary vein anatomy, as well as creation of a surrogate geometry. In an effort to decrease ionizing radiation associated with AF ablation, an ultrasound-guided surrogate geometry approach is proposed as an alternative to routine CT imaging. Ten patients underwent AF ablation using intracardiac ultrasound for the creation of a surrogate left atrial geometry (CartoSound, Biosense Webster, CA); and ten control-cases who had conventional CT-guided imaging (CartoMerge, Biosense Webster, CA) were matched for age, gender, and type of catheter ablation. Sources of radiation included 1) intraprocedural fluoroscopy (CartoSound: 151 ± 43 mGray*cm^2, CartoMerge: 174 ± 130 mGray*cm^2; p=0.6) and 2) CT ionizing radiation (CartoSound: 0 mSv, CartoMerge 9.4 ± 2.3 mSv/CT scan.) When comparing clinical success rates after a trial of previously ineffective anti-arrhythmic drugs, ultrasound-guided AF ablation was non-inferior to a CT-guided approach. This potentially obviates the need for CT-guided imaging, therefore reducing doses of ionizing radiation by nearly 10 mSv per AF catheter ablation.
Correspondence to: Komandoor Srivathsan MD, Division of Cardiology, Mayo Clinic, 5777 East Mayo Boulevard, Phoenix, AZ 85054
With the rise of catheter ablation to treat drug-refractory atrial fibrillation (AF), there is a collective initiative to improve procedural efficiency while increasing safety margins.1,2 Due to a growing concern of cancer risks surrounding ionizing radiation, it is paramount to consider the amount of ionizing radiation associated with AF catheter ablation, particularly with the increasing trend towards serial ablations.2 While the degree of cancer risk associated with radiation exposure is arguably theoretical, the ALARA (As Low as Reasonably Achievable) principle favors seeking alternatives to safely reduce ionizing radiation exposure.3-4
The major source of ionizing radiation surrounding AF ablation is pre-ablation computed tomography (CT) imaging, with a minor contribution from intra-procedural fluoroscopy. Conventionally, impedance or electroanatomic atrial mapping to enable surrogate geometry creation and pulmonary vein (PV) electrical isolation is aided by pre-ablation CT scans. Caveats surrounding CT imaging include its contraindications (i.e. contrast dye allergy), lower sensitivity for detecting left atrial (LA) thrombus, and inability to provide real-time images during ablation. Although magnetic resonance imaging is an alternative, its limitations include cost, time for image acquisition, and contraindication for use with pacemakers.
Reducing effective doses of ionizing radiation from CT imaging may be accomplished by performing catheter ablation guided only by intracardiac echocardiography (ICE). ICE is being recognized as an alternative for creation of surrogate geometry instead of point-to-point electroanatomic mapping.5 In addition to being used for image integration to create a real-time surrogate LA geometry, ICE can also assess pulmonary veins with two-dimensional imaging and Doppler. ICE enables catheter ablation without the cost and time of additional imaging, and without additional ionizing radiation associated with a CT-guided approach to AF ablation. This study proposes the use of ultrasound-guided AF ablation as an alternative to CT-guided imaging, while examining novel ways to decrease ionizing radiation associated with AF ablation.
This is a retrospective study looking at 10 patients who underwent ultrasound-guided (CartoSound) AF ablations at our center. Ten case-controls were subsequently selected, all of whom received pre-ablation CT scans (CartoMerge). Cases were matched for age, gender, and type of catheter ablation (wide-area catheter ablation versus pulmonary vein isolation.) CT imaging was performed using a 64-slice CT scanner. Total radiation doses were collected for each CT scan performed as well as for intra-procedural fluoroscopy when available.
In addition to doses of ionizing radiation, additional outcomes included atrial fibrillation recurrence and short-term complications associated with AF catheter ablation in both groups. AF recurrence was determined after 90-day blanking period following a trial of previously ineffective anti-arrhythmic drugs (AADs), and was based on clinical symptoms, pacemaker or electrocardiographic documentation of AF. Statistical analysis included student T-test or chi-squared analysis.
The Mayo Clinic Arizona Institutional Review Board evaluated the study protocol and determined the study to be exempt from further review, waiving the requirement for informed consent.
While the CartoSound and CartoMerge groups were matched for age, gender, and type of catheter ablation, their baseline characteristics differed when comparing duration of AF (8.7 vs. 3.2 years, p=0.06) and number of previously attempted anti-arrhythmic drugs (2.3 vs.1.3 AADs, p=0.02). There were no significant differences between baseline comorbidities Table 1. Coronary artery disease was defined by evidence of obstructive lesions >50% or prior coronary interventions. Pulmonary disease was defined as reactive airway disease, asthma, or obstructive sleep apnea, regardless of treatment status. The rate of clinical recurrence of AF was similar between the 2 groups (40% vs. 40%, p=0.37), after a trial of previously ineffective anti-arrhythmic drugs Table 2.
Table 1. Baseline Characteristics
|
CartoSound (n=10) |
CartoMerge (n=10) |
p value |
| Age (years) |
63.5 |
62.6 |
ns |
| Male Gender (# patients) |
7 |
7 |
ns |
| Duration AF (years) |
8.7 ± 9.6 |
3.2 ± 3.6 |
0.06 |
| Permanent AF (# patients) |
2 |
4 |
ns |
| Anti-arrhythmic Drug (#) |
2.3 ± 1.1 |
1.3 ± 0.7 |
0.02 |
| LA vol Index (cc/m^2) |
42.0 |
40.6 |
ns |
| Prior ablation (# patients) |
5 |
5 |
ns |
| BMI (kg/m^2) |
31.9 ± 3.2 |
31.9 ± 3.2 |
ns |
| Hypertension (# patients) |
7 |
5 |
ns |
| Diabetes (# patients) |
1 |
3 |
ns |
| Dyslipidemia (# patients) |
7 |
4 |
ns |
| Cardiomyopathy (# patients) |
0 |
3 |
ns |
| Coronary disease (# patients) |
2 |
3 |
ns |
| Pulmonary disease (# patients) |
3 |
2 |
ns |
AF=atrial fibrillation, BMI=body mass index, LA vol=left atrial volume, ns=not significant
Table 2. Procedural Characteristics and Outcomes
|
CartoSound (n=10) |
CartoMerge (n=10) |
p value |
| WACA |
8 |
8 |
ns |
| Duration CA (minutes) |
269.5 |
252.3 |
ns |
| Mitral Line Ablation |
0 |
8 |
|
| Roof Line Ablation |
0 |
4 |
|
| Accessory PV Ablation |
0 |
4 |
|
| CTI ablation |
10 |
10 |
ns |
| Prophylactic AAD at DC |
5 |
5 |
ns |
| Days of follow-up |
110 ± 20 |
219 ± 10 |
0.005 |
| Recurrent AF |
4 |
4 |
0.37 |
AAD=anti-arrhythmic drug, AF=atrial fibrillation, CA=catheter ablation, CTI=cavotricuspid isthmus, DC=post-procedural hospital discharge, PV=pulmonary vein, WACA=wide area catheter ablation
There was no radiation exposure in the CartoSound group outside of intraprocedural fluoroscopy. Radiation from fluoroscopy with CartoSound was not significantly different from CartoMerge (151±43 vs. 174 ± 130 mGycm^2, p=0.6) Figure 1. In the CartoMerge group, patients received pre-ablation CT scans with an average radiation dose of 8.9 ± 2.3 mSv per scan.
Figure 1. Fluoroscopy Dose Area-Product: Fluoroscopy is a minor contributor to overall ionizing radiation associated with atrial fibrillation ablation. There is no significant difference in intra-procedural radiation from fluoroscopy between ultrasound-guided imaging (CartoSound) and conventional CT-imaging (CartoMerge) (p=0.6)
Medical imaging procedures are gaining recognition as an important source of exposure to ionizing radiation in the United States, potentially resulting in high cumulative effective doses.6 While it is difficult to extrapolate cancer risks from large population-based studies and apply them to individual patients, every effort should be made to decrease levels of ionizing radiation when possible.
The primary aim of this study was to increase awareness of how much ionizing radiation is associated with each AF ablation. Measuring actual radiation doses (not estimates), we found that case–controls at our institution were receiving nearly 10 mSv per pre-ablation CT scan. Assuming that an average posterior and lateral chest x-ray is 0.10 mSv, this is equivalent to almost 100 chest x-rays.3 While the attributable cancer risk can only be inferred from existing studies of large epidemiologic proportions, as outlined by the BEIR VII registry,7 a cumulative radiation dose of 19.4 mSv in a population of radiation workers translated into an excess risk ratio of 0.97.8 With current practice favoring serial AF ablations, three AF ablations could theoretically result in 30 mSv of cumulative radiation.2 In these cases, organ equivalent doses to specific tissues such as breast and lung are even higher potentially increasing the lifetime attributable risks of cancer.9
The approach to decreasing ionizing radiation associated with AF is two-fold. The first goal is to assess ways to decrease ionizing radiation associated with pre-ablation CT scans. Beginning with the patient, diligence in ensuring IV site integrity is paramount, and would have prevented extravasation of contrast dye in one patient who received twice the dose of ionizing radiation following a failed CT study. Additionally, reviewing CT images revealed that some patients had a field of view (FOV) extending as far inferiorly as the diaphragm. Recognizing that an extended FOV increased radiation exposure without clinical merit, we limited FOV to focus on just the left atrium and the pulmonary veins. In further consultation with our radiology department, additional technical adjustments were made to the CT scanner that reduced ionizing radiation to nearly 2 mSv per pre-ablation CT scan, without compromising imaging objectives. As techniques evolve to reduce radiation by adjusting CT imaging protocols, a plan to reinforce these protocols is paramount, as is now being done at our institution.
The second approach is to find alternative imaging modalities that reduce or eliminate ionizing radiation. This feasibility study suggests an alternative approach to CT-guided AF ablation by demonstrating non-inferiority of an ultrasound guided method. The use of ultrasound-guidance safely eliminates the need for CT scans, which in turn eliminates the major source of radiation associated with catheter ablation. While this is only a feasibility study, rates of clinical freedom from AF (after a trial of previously ineffective AADs for 120 days) were similar between the 2 groups, and neither group had short-term adverse events within the first 30 days post-procedure.
In addition to a small sample size, there are several other limitations to this study. Baseline characteristics between the two groups were not identical, as the CartoSound group had a longer duration of AF and had been tried on more AADs prior to ablation. Additionally, there were differences in ablation technique between the 2 groups; the CartoSound group had fewer linear line ablations, which may have resulted in increased pro-arrhythmic potential. Additionally, there is a learning curve associated with performing ICE-guided catheter ablation.
While there are several approaches that can be used to decrease ionizing radiation doses associated with AF ablation, an ultrasound-only guided approach may emerge as a solution to moderate radiation doses associated with protocol-driven CT imaging.
With the rising concern of cumulative ionizing radiation exposure associated with medical imaging procedures, we address the sources of radiation associated with atrial fibrillation ablation. Pre-ablation computed tomography scans are a major source of radiation exposure, and are routinely performed on patients undergoing catheter ablation. We demonstrate the potential use of ultrasound-guided catheter ablation as an alternative to CT-imaging.