Diagnostic Tools to Assess Dysfunction of Autonomic Control of the Heart
Richard Sutton1
1Cardiac Dept., Hammersmith Hospital Campus of National Heart & Lung Institute,
Imperial College, London, United Kingdom.
The most important diagnostic tool available in assessment of dysfunction of the autonomic control of the heart is the clinical history which must be taken in the greatest possible detail including from the patient and witnesses of the syncope/event. Correct history taking will make many diagnoses avoiding need for further testing and guide further investigation if needed and when appropriate. This paper focusses on the investigation of patients when required, the available tests, their indications, how to perform them for maximum yield and how to interpret the results. Tilt-testing, carotid sinus massage, active stand, cardiovascular autonomic nervous system tests, ambulatory blood pressure and insertable ECG loop recorder are covered.
Key Words : Cardiovascular Autonomic dysfunction, Syncope, Tilt-testing, Carotid Sinus massage, Active Stand, Ambulatory blood pressure, Insertable ECG loop recorder.
Correspondence to: Professor. Richard Sutton
Cardiac Dept, Hammersmith Hospital, Imperial College,
Ducane Road
London W12 0NN
United Kingdom
Dysfunction of autonomic control of the heart is common and increasingly so in older populations and in some young females. However, the most frequent transient dysfunction or exaggerated normality is a phenomenon known as vasovagal syncope. In this condition, between attacks, there is usually nothing abnormal to detect.
Those physicians interested in autonomic control of the heart employ a panoply of tools to assess their patients' diagnosis, level of disability and prognosis as far as is possible (Table 1). This review will cover all the routinely used tools including indications for their use, practicalities of application and results of the tests.
Table 1. Investigative tools
|
Clinical history - Essential in all.
|
|
Tilt-testing - indicated in many with Vasovagal syncope, Orthostatic hypotension, Postural Orthostatic Tachycardia Syndrome and Psychogenic pseudosyncope.
|
|
Carotid sinus massage - indicated for syncope over the age of 40 years.
|
|
Active stand test - indicated for diagnosis of Classical Orthostatic hypotension
|
|
Cardiovascular Autonomic nervous system tests: Valsalva maneuver, deep breathing test indicated in all with Orthostatic hypotension and others presenting syncope where autonomic dysfunction is suspected.
|
|
Others not covered as not routinely used and some have little relevance to the diagnosis of syncope: cold pressor test, heart rate variability, sweat test, exercise test, catecholamine levels.
|
|
Ambulatory blood pressure - valuable in Orthostatic hypotension and other autonomic dysfunctions to reveal non-dipping and reversed dipping blood pressure requiring i individual management.
Insertable/implantable ECG loop recorder - in all where arrhythmia including reflex- induced arrhythmia is suspected.
|
Clinical History
Every patient requires full history, physical examination, 12-lead ECG and supine and erect, after 3 minutes, blood pressure. This is the so-called initial assessment 1,2. This assessment, especially the history from the patient and witness, is the most important tool that we have with all the other tools are of minor importance in comparison 3. More detailed discussion of symptoms and their timing in relation to the evolution of an episode of syncope is available in the European Society of Cardiology (ESC) Practical Guidelines 2.
Findings at this assessment will guide selection of subsequent diagnostic/assessment tools to be used. By way of examples, the history will often reveal vasovagal syncope (VVS), physical examination may show evidence of heart disease or 12-lead ECG indicate a channelopathy. When the presentation has been syncope and this remains unexplained by the initial assessment, physicians may proceed to tilt-testing or to an Insertable/implantable ECG loop recorder (ILR) which is strictly not an autonomic test but it may provide useful information. Other findings will direct the investigator in other directions , for example, if there is evidence of structural heart disease an echocardiogram will usually be necessary 3.
The available tests are Tilt-testing, Active Stand test, Carotid Sinus Massage, Autonomic Function tests (including, here, only those most practical and informative: Valsalva maneuver, Deep breathing test), Ambulatory blood pressure and ILR. Indications for and performance of these tests and their interpretation will be discussed in this order.
Tilt testing was introduced in 1986 for assessment/diagnosis of unexplained syncope 4. It has evolved much since that time. There has been considerable agreement on the protocol to be employed in Europe, known as the Italian protocol 5, although less so in the United States (US) where isoproterenol may still be used despite its expense. Both continents' Guidelines on syncope classify Tilt-testing as Class IIA for investigation of syncope 1,2,6. Tilt-testing now has many indications, Table 2.
Table 2. Indications for tilt-testing
|
- diagnosis of VVS;
|
|
- confirmation of diagnosis of VVS for patient education about symptom recognition;
|
|
- Education of VVS patient on physical counter-pressure maneuvers;
|
|
- diagnosis of Orthostatic Hypotension (OH) and delayed OH;
|
|
- diagnosis of Postural Orthostatic Tachycardia Syndrome (POTS);
|
|
- diagnosis of Psychogenic Pseudosyncope (PPS).
|
Tilt-testing is also used in research to better understand mechanisms responsible for VVS, OH, POTS and PPS. Such better understanding is aimed at better treatment options presently lacking in our armamentarium. All indications discussed are mostly Class IIa recommendations and none reaches Class I in Guidelines 1,2,6.
Protocols for tilt-testing are relatively consistent between centers. The patient is asked to fast for a short time prior to the test (~2 hours) but take normal medications except those with cardiovascular activity which are advised not to be taken on the day of the test. On arrival or before, the purpose of the test, usually to achieve a diagnosis, is explained to the patient which includes the possibility of induction of syncope. Patients are advised to come accompanied as they may need some support in travelling home. The patient may be asked to sign a consent form although this not considered essential everywhere.
If the patient is already known, the medical records will be consulted so the staff performing the test understand what may be expected and what information is required from the test. If the patient is not already known, a full history will be taken and the referring information carefully scrutinized. The test is not usually performed by a physician, more often by a nurse suitably qualified, a technologist or physiologist. Rapid access to resuscitation equipment is a requirement when the test is performed, plus ready availability of a physician with knowledge of tilt-testing.
The patient is asked to lie supine on the tilt-table where the monitoring equipment will be placed, ECG and a device for recording beat-to-beat blood pressure (BP) and straps to support the patient in the event of syncope. This is considered essential as otherwise valuable data will be lost. It is impossible to achieve repeated cuff sphygmomanometry in under 40s per measurement.
Once everything is ready, the patient remains in the supine position for 5-10min. This should be longer (arbitrarily 20min is selected) if venous or arterial lines are placed. The reason for this is that any pain caused will undoubtedly alter the patient's autonomic atmosphere which must be allowed to settle.
The table is tilted to a 60-700, head up position that is near vertical but insufficient to bring into play the muscle activity in the legs when standing erect. Thus, this position permits substantial blood pooling in the legs in addition to that in the abdomen and pelvis occurring on standing. The staff are required to check that patients do not move their legs which would oppose the blood pooling therein. The patient is allowed to rest in this position without speaking except when questioned as to symptoms. The lights of this quiet room are often dimmed to promote tranquility.
Monitoring of ECG and BP is closely watched by the staff. Events such as tilt-up, symptoms especially palpitations, dizziness, evidence of a prodrome, moment of loss of consciousness (LoC) are recorded in the monitoring system. In VVS, the blood pressure always falls first and several minutes before cardioinhibition occurs 7. When BP is <90mmHg prodromal symptoms begin and LoC usually occurs when BP is <60mmHg. LoC is denoted by head-flop (EEG, if recorded, will show slow waves or be completely flat) and will be a very important event to correlate with the BP and HR as if it occurs substantially before asystole it is unlikely that treating the bradycardia with a pacemaker will be helpful 8.
If the patient appears about to lose consciousness with a fall in BP and heart rate (HR) questions are asked about symptoms. The test may be terminated before final loss of consciousness but more usually complete loss of consciousness is required for a clearly positive test. It is important to be equipped with a table that tilts down to supine quickly (<15 seconds) as a slow tilt-down promotes extended periods of unconsciousness which is unpleasant and possibly dangerous 9.
Thus, a positive test displays the hemodynamic patterns described here together with LoC but what is most important in interpretation is that on recovery the patient states that this induced attack reproduces what has happened previously, the spontaneous attack. If there is no reproduction of symptoms the test should be considered negative or 'false' positive. In a large group of normals without previous syncope, syncope occurred in approximately 13% 10. These normals could be considered false positive or, perhaps, revealing a hypotensive susceptibility which is very common in the population (~40%) 11. Early studies of vasovagal syncope (VVS) revealed that almost any fit and healthy person can sustain VVS if enough blood volume is withdrawn 12
Once the patient is supine again recovery is usually prompt and the patient can be questioned on what has been experienced. Some patients, more at older age (>60 years), will deny loss of consciousness signifying amnesia for the event 13. This must be recorded as it is pertinent to falling as any falls may be consequent on syncope 1.
If nothing happens the passive part of the test runs for 20 minutes at which time 300-400 mcg of nitroglycerine spray is administered sublingually. This is the description of the Italian protocol 14.
Nitroglycerine delivers additional blood pooling in the peripheral circulation increasing the likelihood of syncope. It may cause a transient headache but appears not to disturb sensitivity or specificity of the test 5. This drug phase lasts 15min without tilt-down before drug administration. A positive test in this phase manifests in the same way as in the passive phase.
In the US, isoproterenol has been used as a drug challenge (protocols vary). However, this drug requires IV access, is now expensive, has more side-effects than nitroglycerine and has some hazards including induction of ventricular tachyarrhythmias or myocardial ischemia. The dose of isoproterenol is typically 2 mcg/min but may be increased to obtain a heart-rate response of 120 bpm. At the end of the passive phase tilt-down is usually practiced before tilt-up again as the infusion is having its required effect 6.
If a test is negative, no conclusion can be drawn; VVS is not eliminated from possible diagnoses, which still may be made from the history 1.
Positive tests may be classified according to the manner of collapse 14. The Vasovagal international study (VASIS) group hoped that collapse, be it mixed bradycardia and vasodepression (VASIS I), or dominantly cardioinhibition (VASIS IIA solely bradycardia or VASIS IIB asystole) or dominantly vasodepression (VASIS III) would be reproducible in a given patient, reproduce what happens in spontaneous attacks and point to an appropriate therapy. Unfortunately, none of these is the case 14. It is a surprising that the classification continues to be widely used. It remains, however, a shorthand for how the collapse occurred on the occasion of the test. Figure 1 shows VASIS type IIB positive tilt test.
Figure 1. VASIS IIB Cardioinhibitory Positive Tilt-test.
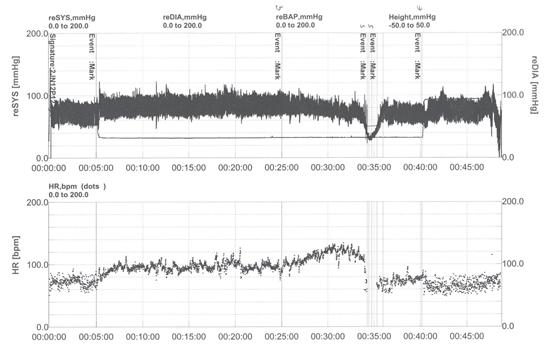
shows in the upper panel beat-to-beat blood pressure (BP) recording from a finger
photoplethysmographic device as (SYS) (range 0-200 mmHg) and in the lower panel heart rate
(HR) (range 0-200 bpm). Time in minutes is shown at the bottom of each panel. The test begins
with the supine phase. At event mark 1, the patient is tilted up to 600, BP and HR rise initially, there
follows a stable phase. At event mark 2, nitroglycerine 400 mcg is administered sublingually with
the effect of BP reduction and HR rise. At event mark 3, patient was dizzy and BP collapsed steeply
with a modest fall in HR preceding this BP fall. At maximum BP fall to 40mmHg the patient lost
consciousness with 5 seconds of asystole (not well seen at this recording speed) and was tilted
down, event mark 4. The patient recovered consciousness at event mark 5. This is classified as
VASIS IIB severely cardioinhibitory tilt positive.
The timing of the positivity appears to suggest a more severe situation when it occurs in the passive phase but this has received rather little attention. The severity of the attack induced is much in the hands of the operators as the longer the patient is pushed into the evolution of the attack, delay in tilt-down and slow tilt down, the more severe it will be 9.
In contrast to VVS, where attacks develop after some minutes (>3) of tilt, OH begins immediately even in delayed OH Figure 2 but, in this latter condition, it only reaches diagnostic criteria 16 later than 3min 17. Classical OH is defined as a sustained decrease in systolic blood pressure 20 mmHg and/or diastolic blood pressure 10 mmHg, within 30s 16. Delayed OH, first described by Streeten and Anderson,1992 18, has limited available data on its pathophysiology and its differences from classical OH. A recent study has shown, however, that it may be more common than classical OH, occurring more often in males, older and Parkinsonian patients but with less profound hypotension 17. OH patients develop symptoms gradually and few have full syncope but more-often pre-syncope.
Figure 2. Classical and Delayed Orthostatic Hypotension on Tilt.
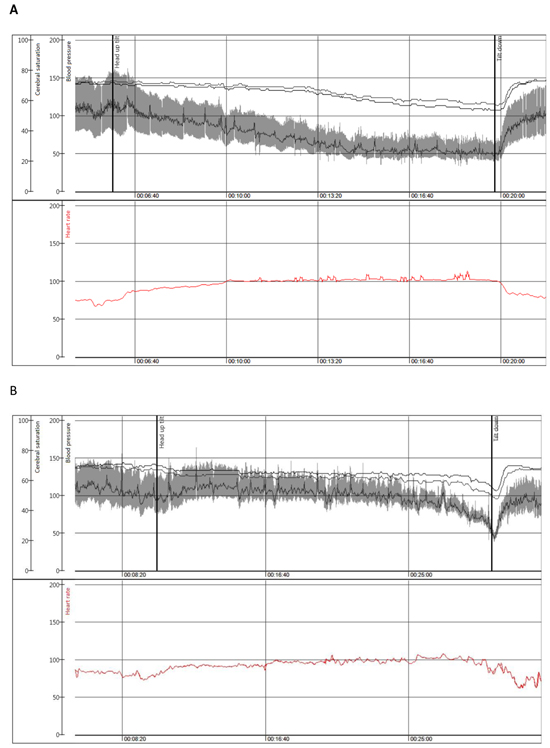
shows in panel
A: Beat to beat blood pressure (mmHg) from a photoplethysmographic finger device
and heart rate (beats/min) in upper section with cerebral saturation (%) from a near-infra-red
spectrum device in the lower section during head-up tilt in a female patient aged 50 years with
classical orthostatic hypotension.
Panel
B shows, in a similar format to Panel
A: Delayed orthostatic hypotension leading ultimately
to vasovagal reflex in a male patient of 80 years. Reproduced with permission of Frontiers
Cardiovascular Medicine.
POTS is clearly demonstrated on tilt Figure 3, although tilt may not be necessary for diagnosis 19. On tilt, a rapid acceleration of heart rate from the elevated rate at rest. The rise peaks and tends to stabilize by 10 minutes of tilt and there will be no fall in BP that might meet criteria for OH. POTS is a clinical syndrome and tilt-table data form part of the diagnosis. For a correct diagnosis, a HR rise, in adults, of >30 bpm without hypotension on the adoption of the erect posture is required 20. These defined rate criteria alone, however, do not conclude a diagnosis without the clinical features of the syndrome 21.
Figure 3. Postural Orthostatic Tachycardia Syndrome on Tilt.
Carotid Sinus Massage (CSM): CSM is indicated in all patients presenting syncope over the age of 40 years (abnormalities of CSM are extraordinarily rare below this age). CSM should be, if possible, combined with tilt-testing as it can be performed in the secure environment of the tilt laboratory with invaluable monitoring of HR and BP and allow its repeat in the erect position permitting more diagnoses to be made 1. In most cases, a physician is required to perform CSM which can be made either before or after the tilt test. Usually, right carotid massage in the supine position is made first, followed by left CSM in supine then right followed by left CSM in the upright position (same angle as tilt-testing). The carotid artery is identified in its position with maximal pulsation lateral to the cricothyroid cartilage, medial to the angle of the jaw and in front of the anterior border of the sternocleidomastoid muscle. The patient's face is rotated away from the operator. Ten seconds massage at moderate pressure, insufficient to occlude the artery, is made at this point by moving the operator's 2nd, 3rd and 4th fingers up and down the course of the artery. The ECG must be visible to the operator who may cease massage if asystole is established. CSM is contraindicated in patients with known severe carotid stenosis because of possible embolism of plaque to the brain and ensuing stroke although this is rare and of the order of 0.24% of massages1. It has been said that a finding of carotid bruit is a contraindication to CSM but as bruit audibility is not correlated with severity of carotid stenosis this contraindication has received less importance. Figure 5 illustrates a positive CSM. The patient’s symptoms are recorded as a positive test is a combination of bradycardia, blood pressure fall and reproduction of previous symptoms. A positive result may be hypotension, systolic BP fall >50 mm Hg alone (vasodepression), intense bradycardia/asystole (cardioinhibition), asystole >6 seconds or a mixture of the two (mixed) with asystole <3 seconds. Administration of IV Atropine (0.02mg/Kg) is known as the 'Method of symptoms', after a positive cardioinhibitory or mixed test atropine will eliminate the vagal slowing of the heart and allow assessment of the likely BP fall and symptoms, if cardioinhibition is later opposed by an implanted pacemaker. This was recently reviewed in a large case series 23. It must be emphasized that such findings without symptoms are far less important in diagnosis and decision making as the diagnosis is then carotid sinus hypersensitivity (CSH) and not carotid sinus syndrome. The prognosis and management of CSH is not well understood 24.
A mixed form of carotid sinus syndrome diagnosed by carotid sinus massage (CSM) performed according to the 'method of symptoms'. Upper panel: CSM was performed during beat-to-beat, electrocardiographic (top trace) and systolic blood pressure monitoring (bottom trace) with the patient on a tilt table in the upright 60° position. Arrows indicate the time of beginning and end of massage, which was continued for 10s. A 9.6s asystole was induced soon after the beginning of the massage with symptom reproduction. The mean circulatory filling pressure decreased to <40 mmHg after 10 seconds of CSM; this was insufficient to preserve brain perfusion resulting in syncope. Lower panel (Atropine IV): In order to determine the relative contribution of the two components of the reflex, the cardioinhibitory component was suppressed by means of IV infusion of 0.02 mg/kg atropine and CSM was repeated. Systolic blood pressure fell to ~75 mmHg and the patient again had syncope after approximately 15 seconds. The vasodepressor component of the reflex and the asystolic reflex were both major determinants of syncope in this patient justifying classification as Mixed form3. Reproduced with permission of European Society of Cardiology.
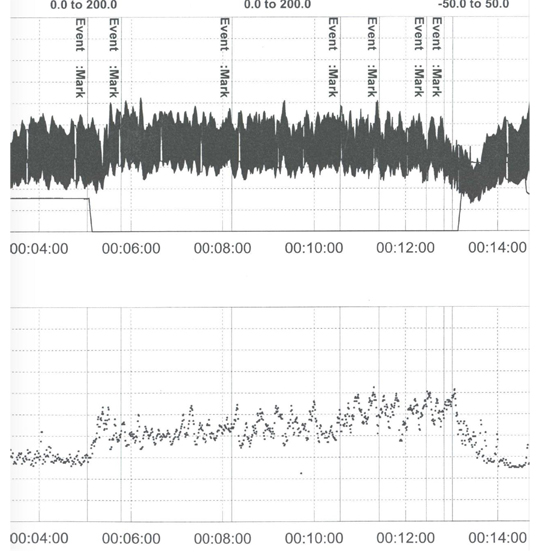
Figure 4. Psychogenic Pseudosyncope on Tilt.
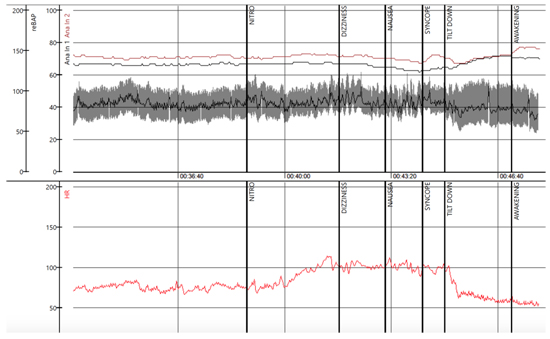
Figure 5. Carotid Sinus Massage and 'Method of Symptoms'.
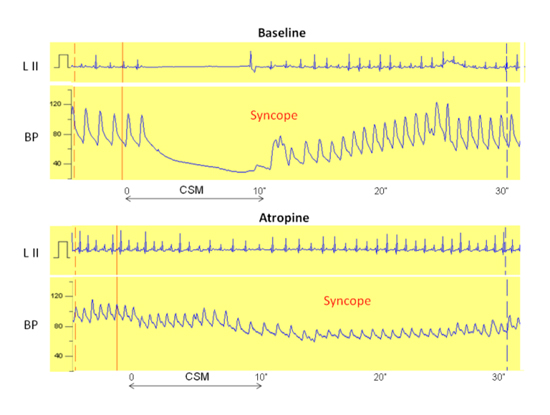
A mixed form of carotid sinus syndrome diagnosed by carotid sinus massage (CSM) performed
according to the 'method of symptoms'. Upper panel: CSM was performed during beat-to-beat,
electrocardiographic (top trace) and systolic blood pressure monitoring (bottom trace) with the
patient on a tilt table in the upright 60° position. Arrows indicate the time of beginning and end
of massage, which was continued for 10s. A 9.6s asystole was induced soon after the beginning
of the massage with symptom reproduction. The mean circulatory filling pressure decreased to
<40 mmHg after 10 seconds of CSM; this was insufficient to preserve brain perfusion resulting
in syncope. Lower panel (Atropine IV): In order to determine the relative contribution of the two
components of the reflex, the cardioinhibitory component was suppressed by means of IV infusion
of 0.02 mg/kg atropine and CSM was repeated. Systolic blood pressure fell to ~75 mmHg and the
patient again had syncope after approximately 15 seconds. The vasodepressor component of the
reflex and the asystolic reflex were both major determinants of syncope in this patient justifying
classification as Mixed form3. Reproduced with permission of European Society of Cardiology.
This test differs from Tilt by enforcing use of the leg muscles to maintain the unsupported upright posture which secondarily involves the leg muscle pump increasing venous return and opposing blood pooling in the lower limbs. There are other differences, notably the patient should be standing without support which may not be possible or safe in some of the patients who are candidates for the test. Further, it is not possible in many candidates to pursue such a test for up to 35 minutes (Italian protocol 5) as is done without inducing intolerance in the vast majority of those who undergo tilt tests. Normally, this test is continued for 3 minutes to ascertain if the criteria for classical OH are met and manual BP measurement is used. If this test were to be more useful and widely adopted it should be performed for longer (>10 minutes) and with the full monitoring of BP and ECG used in tilt testing. It is difficult to see that this will happen given the tolerance issues mentioned above.
This test is not covered in any detail in recent guidelines 1,2,6. At present, it is recommended for assessment of classical OH in the clinic setting where it is a simple and practical part of the initial assessment. Patients presenting syncope or dizziness on standing after exercise or meals or in hot weather without any reflex features such as sweating or nausea will be those for whom the Active Stand test will be most valuable. On the test, If a patient becomes symptomatic with BP fall, within 3 minutes, of 20 mm Hg systolic, the importance of the diastolic pressure appears to be less 25, diagnosis of classical OH is confirmed. If BP fall of the same degree occurs without symptoms classical OH is likely and may be confirmed by tilt-test. In the European guidelines 1,2, the Active Stand as part of the initial assessment and is Class I, so also in the North American version 6. POTS could also be diagnosed by Active Stand but 10 minutes is required which is much less likely to be tolerated. In Classical OH associated with primary autonomic failure there will be no response of heart rate to the upright position but, in secondary forms of Classical OH and delayed OH, the heart rate response is only expected to be attenuated.
Cardiovascular Autonomic Tests
These tests are less frequently performed. It might be supposed that they will routinely be done by neurologists but this is often not the case. Cardiologists attempt to fill this gap but not all are sufficiently motivated toward quality control and full interpretation. The best situation is where an expert in cardiovascular autonomics supervises the laboratory, an all too rare occurrence. The expert will have access to tilt-testing and all the other tests that have been or will be discussed here. As in all other tests the clinical history of very great importance in interpretation of results. Probably, the history will be taken again and may reveal some hitherto unrevealed features and must include documentation of current medication. Patients are asked to fast before coming for about 3 hours and to avoid caffeine-containing drinks on the day of testing. The first test to be performed is the Valsalva maneuver.
The patient is monitored as in tilt-testing and when ready is asked to make a maximal forced expiration for 15 seconds against with closed nose and mouth or, probably better into a closed loop system with 40 mmHg resistance (monitored by a modified sphygmomanometer). This is difficult for patients and staff must be well trained in correctly guiding this maneuver. Beat-to-beat arterial pressure (BP) and heart rate will reveal the hemodynamic events and by inference the state of autonomic control of the heart. Figure 6 shows a normal result compared with that in autonomic failure.
Figure 6. Shows in the left panel a normal Valsalva maneuver and, in
the right panel a patient with autonomic failure where very
limited hemodynamic changes are seen as the necessary reflex
mechanisms are damaged.
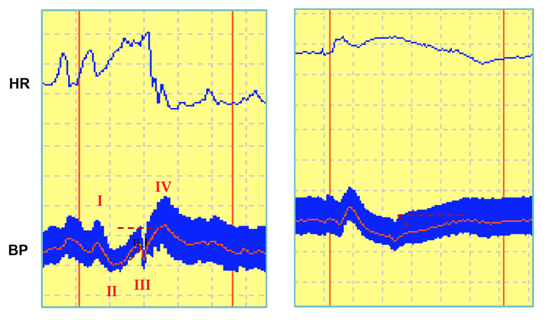
HR=heart rate; BP=blood pressure, I,II,III, and IV indicate the four phases of the normal Valsalva
maneuver. Reproduced with permission of the European Society of Cardiology.
Four phases are described as normal behavior. Phase 1 in first 2-3s the left ventricle has benefitted from the deep inspiration at the commencement of the test and there is an increase in BP. As forced expiration proceeds, in Phase 2, intrathoracic pressure increases, venous return, cardiac output and BP fall prompting a baroreflex mediated heart rate increase. There follows, in Phase 3, marked sympathetic outflow to increase systemic vascular resistance with both of these mechanisms opposing the fall in BP. There is also parasympathetic activity to slow the heart rate. Phase 4 is release of respiratory resistance to expiration resulting in large increase in venous return and cardiac output but systemic vascular resistance falls more slowly and BP briefly rises much (so-called overshoot) while heart rate continues to decline and stabilizes. This is visually readily assimilated and abnormalities of baroreflex function are very clearly apparent.
Other findings may present in the Valsalva maneuver such as in situational syncope where marked hypotension is seen, together with dizziness, in Phase 3, but there is a normal heart rate response.
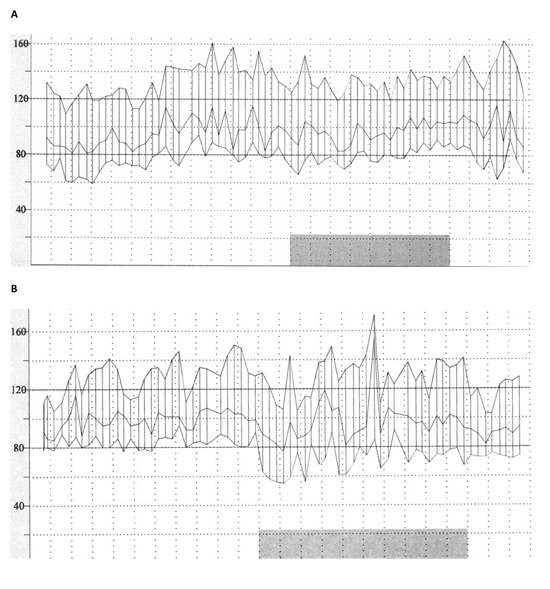
Figure 7. Non-dipping and Reverse-dipping. Figure A shows blood pressure
only from a 24-hour ambulatory blood pressure monitor. Sleep
is marked by the lower dark bar. During this time the expected
BP fall is not present. Figure B shows, in an identical format,
evidence of BP rise during sleep which is Reverse-dipping. Blood
pressure scale is in mmHg. Illustrations courtesy of A Fedorowski.
This test also offers enhanced yield if it is combined with non-invasive beat-to-beat blood pressure and ECG monitoring. The patient is asked to breathe deeply at 6 breaths/s which can best be timed by a metronome over a period of 1 minute. On inspiration, HR rate will increase and decrease on expiration this is sinus arrhythmia demonstrating intact autonomic control. It should be recognized that this is absent in atrial septal defect implying that patients with this condition will show this abnormality without significance in terms of loss of autonomic function. The changes in HR have a primary hemodynamic basis with autonomic modulation. Thus, cardiac output and blood pressure fluctuate in parallel with HR. The effect of deep inspiration increasing venous return by negative intrathoracic pressure drawing blood into the thorax imposes these changes in hemodynamics and HR which are negated by the presence of an atrial septal defect. In this abnormality successful surgery restores sinus arrhythmia. The expected peak to trough variation is >15bpm in patients <50 years and is expected to decline with increasing age.
A normal deep breathing test is associated with sinus arrhythmia. When abnormal there is no sinus arrhythmia, no fluctuation in total peripheral resistance and represents severe autonomic denervation. However, in the abnormal result the hemodynamically driven changes still occur3.
HR=heart rate; BP=blood pressure; CO=cardiac output; TPR=total peripheral resistance; Resp=respiration. Reproduced with permission of Oxford University Press.
24-hour Ambulatory Blood Pressure
This is a test used frequently by hypertension specialists but evidence about autonomic status can also be derived from these recordings. BP is measured usually by cuff every few minutes over 24 hours and is sufficiently accurate to have clinical value. The data is presented in a very clear graphical form Figure 8
So-called dipping of blood pressure during sleep is recognized as a normal phenomenon but lack of dipping or more obviously reverse dipping is abnormal and associated with a reduced prognosis and with Orthostatic Hypotension. These detailed recordings are also able, with good diary keeping, to detect post-prandial hypotension a common finding in patients with OH. The findings of non-dipping, reverse-dipping and post-prandial hypotension are indicative of abnormal cardiac autonomic control.
Insertable/Implantable ECG Loop Recorder
The ISSUE (International Study of Syncope of Unknown Etiology) 2 26 prompted classification of the rhythms seen on insertable/implantable loop recorders in those with clinically defined reflex syncope under consideration for pacing. The steering committee of ISSUE 2 met to debate the recordings received resulting in formal grouping of bradycardias into 2 groups, asystole and bradycardia, tachycardia and no or slight variations in rhythm and rate. These groupings were made for events including syncope, pre-syncope or palpitations that patients either triggered themselves or occurred automatically from the pre-determined set thresholds of the devices. The classification was intended first to help the ISSUE 2 investigators, subsequently offer a clinically useful approach which is relevant to interpretation of a reflex role in the findings 27.
The bradycardias were type 1 asystole divided into 1a: sinus arrest: progressive sinus bradycardia or initial sinus tachycardia followed by progressive sinus bradycardia until sinus arrest, considered to be of probable reflex origin; type 1b: sinus bradycardia plus atrioventricular block (AVB) and ventricular pause associated with slowing sinus rate, also considered to be of reflex origin; type 1c: atrioventricular block of sudden onset associated with ventricular pause and a rise in sinus rate. The latter was considered to be due to ventricular conduction tissue disease. The classification was rigorously followed but to the surprise of the investigators in both ISSUE 2 and ISSUE 3 28 studies approximately 20% of attacks fell into the 1c category. In ISSUE 3, this finding prompted reviewers of the paper to argue that this was occult ventricular conduction tissue disease which was a clear, already established, indication for pacing, thus, devaluing the trial. In ISSUE 3 follow-up of 2 years no patient developed any ECG findings of ventricular conduction tissue disease. Such findings might have been expected given the earlier findings of Brignole and colleagues of progression of conduction tissue disease in an ILR study over 15 months 29. After debate it was accepted that this type 1c could be a form of reflex atrioventricular block. Subsequently, more has been learnt about reflex AV block which has recently been reviewed 30.
In the classification, type 2 bradycardias were defined as decrease in HR>30% or to<40 bpm for >10seconds and were consider of likely reflex origin. Type 3 no or slight rhythm and rate alteration were defined as variations in HR <30% or at a rate >40 bpm. These could not be explained but it seemed likely that if the patient were syncopal there had been, by inference, a reflex vasodepressive attack. Type 4: tachycardias:
4a:progressively rising sinus tachycardia, considered of uncertain cause but could be of reflex origin associated with vasodepression; 4b atrial fibrillation; 4c non-sinus supraventricular tachycardia; 4d: ventricular tachycardia, all 4b,4c, 4d are, of course, cardiac arrhythmias and not obviously reflex in origin but there be a reflex role in initial slowing of the heart rate.
In order to ascertain the mechanism of a syncopal or pre-syncopal episode use of an ILR is the optimal device and it has moved progressively forward in timing of use of investigative tools in recent ESC guidelines 1. In cases of intermediate risk, ILR is now the recommended investigative tool because of the quality of the data allowing reasoned decisions as to management.
The prognosis of diagnostic findings on the tests described is covered in detail in guidelines 1,6. Here, it can be summarized as VVS is considered benign although has been associated with vascular disease in population studies 31. Recurrence is likely over many years. The immediate prognosis following diagnosis of VVS appears quite good 32. Carotid sinus syndrome appears not to be mortal but recurrence is likely 33. Orthostatic hypotension, when primary, has a poor prognosis and, when secondary, is slightly less poor. OH of non-neurogenic origin has been shown in populations to have a poor prognosis 34 with similar findings for non-dipping and reversed dipping patients identified on ambulatory blood pressure recordings 35. POTS has a prognosis of persistence in many patients 21. PPS is difficult to treat but some successes have been reported 22.
The available tests discussed are very helpful for clinicians to determine the underlying cause of their patients' presentations and to some extent assess their prognosis and plan their treatment. Unfortunately, knowledge of prognosis remains incomplete and treatments are not as effective as desired. Of all the tests discussed, tilt-testing is considered the most clinically valuable because of its ease of performance, relatively cheapness, wide coverage of conditions requiring evaluation and importance of diagnoses reached.
-
Brignole M, Moya A, de Langhe FJ, Deharo J-C, Elliott PM, Fanciulli A, Fedorowski A, Furlan R, Kenny RA, Martin A, Probst V, Reed MJ, Rice CP, Sutton R, Ungar A van Dijk JG.2018 ESC Guidelines for the diagnosis and management of syncope. Eur Heart J 2018; 39: 1883–1948. doi:10.1093/eurheartj/ehy037.
- Brignole M, Moya A, de Langhe FJ, Deharo J-C, Elliott PM, Fanciulli A, Fedorowski A, Furlan R, Kenny RA, Martin A, Probst V, Reed MJ, Rice CP, Sutton R, Ungar A, van Dijk JG. Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope. Eur Heart J 2018; e1–e38 doi:10.1093/eurheartj/ehy071.
- Wieling W, van Dijk N, de Lange FJ, Olde Nordkamp LR, Thijs RD, van Dijk JG, Linzer M, Sutton R. History taking as a diagnostic test in patients with syncope: developing expertise in syncope. Eur Heart Journal 2015; 36: 277-280.
- Kenny RA, Ingram A, Bayliss J, Sutton R. Head-up tilt: a useful test for investigating unexplained syncope. Lancet 1986; 1: 1352-1355.
- Bartoletti A, Alboni P, Ammirati F, Brignole M, Del Rosso A, Foglia Manzillo G, Menozzi C, Raviele A, Sutton R. 'The Italian Protocol': a simplified head-up tilt testing potentiated with oral nitroglycerin to assess patients with unexplained syncope. Europace 2000;2: 339-342.
- Shen WK, Sheldon RS, Benditt DG, et al. ACC/AHA/HRS Guideline for the evaluation and management of syncope. Circulation 2017; 136:e25-e59.
- Jardine DL, Wieling W, Brignole M, Lenders JWM, Sutton R, Stewart J. The pathophysiological mechanism of the vasovagal response. Heart Rhythm 2018;15: 921-929.
- Saal DP, Thijs RD, van Zwet EW, et al. Temporal Relationship of Asystole to Onset of Transient Loss of Consciousness in Tilt-Induced Reflex Syncope. JACC: Clin Electrophysiol 2017;3:1592-1598.
- Zysko D, Fedorowski A, Nilsson D, Rudnicki J, Gajek J, Melander O, Sutton R. Tilt-testing results are influenced by tilt protocol. Europace 2016; 18: 1108-1112.
- Petersen ME, Williams TR, Gordon C, Chamberlain-Webber R, Sutton R. The normal response to prolonged passive head up tilt testing. Heart 2000; 84: 509-514.
- Ganzeboom KS, Mairuhu G, Reitsma JB, et al. Lifetime cumulative incidence of syncope in the general population: a study of 549 Dutch subjects aged 35–60 years. J Cardiovasc Electrophysiol 2006;17:1172–1176.
- Wieling W, Jardine DL, de Langhe FJ, Brignole M, Nielsen HB, Stewart J, Sutton R. Cardiac output and vasodilatation in the vasovagal response: an analysis of the classical papers. Heart Rhythm 2016; 13: 798-805.
- O'Dwyer C, Bennett K, Langan Y, et al. Amnesia for loss of consciousness is common in vasovagal syncope. Europace 2011; 13: 1040-1045.
- Brignole M, Menozzi C, Del Rosso A, Costa S, Gaggioli G, Bottoni N, Bartoli P, Sutton R. New classification of haemodynamics of vasovagal syncope: beyond the VASIS classification. Analysis of the pre-syncopal phase of the tilt test without and with nitroglycerin challenge. Vasovagal Syncope International Study. Europace 2000; 2: 66-76.
- Moya A, Brignole M, Menozzi C, Garcia-Civera R, Tognarini S, Mont L, Botto G, Giada F, Cornacchia D, on behalf of the International Study on Syncope of Uncertain Etiology (ISSUE) Investigators. Mechanism of syncope in patients with isolated syncope and in patients with tilt-positive syncope. Circulation 2001;104:1261-1267.
- Freeman R, Wieling W, Axelrod FB, et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res 2011;21:69-72.
- Torabi P, Ricci F, Hamrefors V, Sutton R, Fedorowski A. Classical and delayed orthostatic hypotension in patients with unexplained syncope and severe orthostatic intolerance. Front Cardiovasc Med 2020; 7:21. doi: 10.3389/fcvm.2020.00021
- Streeten DH, Anderson GH, Jr. Delayed orthostatic intolerance. Arch Intern Med. 1992;152:1066-1072.
- Sheldon RS, Grubb BA II, Olshansky B, Shen W-K, Calkins H, Brignole M, Raj SR, Krahn AD, Morillo CA, Stewart JM, Sutton R, Sandroni P, Friday KJ, Hachul DT, Cohen MI, Lau DH, Mayuga KA, Moak JP, Sandhu RK, Kanjwal K. 2015 Heart Rhythm Society Expert Consensus Statement on the Diagnosis and Treatment of Postural Tachycardia Syndrome, Inappropriate Sinus Tachycardia, and Vasovagal Syncope. Heart Rhythm 2015 http://dx.doi.org/10.1016/j.hrthm.2015.03.02P
- Schondorf R, Low PA. Idiopathic postural orthostatic tachycardia syndrome: an attenuated form of acute pandysautonomia? Neurology 1993;43:132–137.
- Olshansky B, Cannom D, Fedorowski A, Stewart J, Gibbons C, Sutton R, Shen W-K, Muldowney J, Chung TH, Feigofsky S, Nayak H, Gall N, Kavi L, Calkins H, Benditt DG. Postural orthostatic tachycardia syndrome (POTS): A critical assessment . Prog Cardiovasc Dis 2020; doi.org/10.1016/j.pcad.2020.03.010
- Tannemaat M, van Niekerk J, Reijntjes R, Thijs RD, Sutton R, van Dijk JG. The semiology of tilt-induced psychogenic pseudosyncope. Neurology 2013; 15:1070-1118.
- Solari D, Maggi R, Oddone D, Solano A, Croci F, Donateo P, Brignole M. Clinical context and outcome of carotid sinus syndrome diagnosed by the 'method of symptoms'. Europace 2014; 16: 928-934.
- Ryan DJ, Steen N, Seifer MC, et al. Carotid sinus syndrome, should we pace? A multicentre, randomized controlled trial (Safepace 2). Heart 2010; 96: 347–351.
- Fedorowski A, Hamrefors V, Sutton R, van Dijk G, Freeman R, Lenders J, Wieling W. Do we need to evaluate diastolic blood pressure in patients with suspected orthostatic hypotension? Clin Auton Res 2017; 27: 167–173. DOI 10.1007/s10286-017-0409-77
- Brignole M, Sutton R, Menozzi C, Garcia-Civera R, Moya A, Wieling W, Andresen D, Benditt DG, Vardas P for the International Study on Syncope of Uncertain Etiology [ISSUE 2] Group. Early application of an implantable loop recorder allows effective specific therapy in patients with recurrent suspected neurally mediated syncope. Eur Heart J 2006; 27: 1085-1092.
- Brignole M, Moya A, Menozzi C, Garcia-Civera R, Sutton R. Proposed electrocardiographic classification of spontaneous syncope documented by an implanted loop recorder. Europace 2005; 7: 14-18.
- Brignole M, Menozzi C, Moya A, Andresen D, Blanc JJ, Krahn AD, Wieling W, Beiras X, Deharo JC, Russo V, Tomaino M, Sutton R. Pacemaker therapy in patients with neurally-mediated syncope and documented asystole. Third international study on syncope of unknown etiology (ISSUE-3): a randomized trial. Circulation 2012; 125: 2566-2571.
- Brignole M, Menozzi C, Moya A, Garcia-Civera R, Mont L, Alvarez M, Errazquin F, Beiras J, Bottoni N, Donateo P on behalf of the International Study on Syncope of Uncertain Etiology (ISSUE) Investigators. Mechanism of syncope in patients with bundle branch block and negative electrophysiological test. Circulation 2001; 104: 2045-2050.
- Sutton R. Reflex atrioventricular block. Front Cardiovasc Med 2020; DOI: 10.3389/fcvm.2020.00048
- Ricci F, Manzoli L, Sutton R et al. Hospital admissions fororthostatic hypotension and syncope in later life: insightsfrom the Malmo Preventive Project. J Hypertens 2016; doi:10.
1097/HJH.0000000000001215.
- Pournazari P, Sahota I, Sheldon R. High remission rates in vasovagal syncope: systematic review and meta-analysis of observational and randomized stu- dies. JACC Clin Electrophysiol 2016. http://dx.doi.org/10.1016/j.jacep 2016.10.012.
- Brignole M, Menozzi C, Lolli G, Bottoni N, Gaggioli G. Long-term outcome of paced
and nonpaced patients with severe carotid sinus syndrome. Am J Cardiol 1992;69:
1039–1043.
- Ricci F, De Caterina R, Fedorowski A. Orthostatic Hypotension: Epidemiology, Prognosis, and Treatment. J Am Coll Cardiol. 2015;66(7):848-60.