Sixty consecutive patients who suffered from drug-refractory symptomatic paroxysmal atrial fibrillation (PAF) underwent PVI by means of second-generation CB. After isolation of each PV, a systematic evaluation was conducted to evaluate their potential contribution of loss in vagal innervation by using ECVS, retrospectively. The exclusion criteria were any contraindications for the procedure, including the presence of an intracavitary thrombus, uncontrolled heart failure, contraindications to general anaesthesia and prior AF ablation. All patients signed informed consent for the procedure. The ethical committee of our institution approved the study. The protocol was carried out in accordance with the ethical principles for medical research involving human subjects established by the Declaration of Helsinki, protecting the privacy of all participants as well as the confidentiality of their personal information.
A transthoracic echocardiogram was performed within 1 week prior to ablation enabling assessment of structural heart disease. To exclude the presence of thrombi, trans-oesophageal echocardiography was performed the day before the procedure. All patients underwent a pre-procedural computed tomography scan to assess detailed left atrial (LA) and PV anatomy. All antiarrhythmic drugs (AAD) were discontinued at least 3 days before ablation, apart from amiodarone that was stopped 1 month before. Procedures were performed under general anesthesia and atropine was prescribed.
The heart rate, blood pressure, oximetry, plethysmography, patient and room temperature, capnography and respiratory gases were monitored continuously throughout the procedure. If patients were in AF at the beginning of the procedure, an external cardioversion was executed to restore sinus rhythm. Then through the right femoral vein, a quadripolar catheter was advanced to the right internal jugular vein in the region of the jugular foramen, being directed medially, to perform ECVS. Once correct position was achieved, a direct current stimulation with square wave pulses of 50 microseconds in duration at a frequency of 50 Hz, and amplitude (adapted according to patient characteristics, 0.5 to 1 V/kg limited to 70 V) between 50 to 70 V was delivered through a conventional catheter in order to observe the patient basal VR. Short stimulations and minor modifications were performed to look for the optimal position corresponding to the highest response of sudden cardioinhibition. After having identified the ideal stimulating position, 5 s of stimulation was delivered.The catheter was held in this position for vagal stimulation during all the procedure. Immediately after achieving isolation in each PV, ECVS was repetated. All ECVS responses were recorded as was the duration and type of vagal response induced in each following stimulation. Then, through a single transseptal puncture, an inner-lumen mapping catheter (Achieve®, Medtronic©) was advanced to each PV ostium through a steerable 15 Fr sheath (FlexCath Advance®, Medtronic©, Minneapolis, MN, USA). Baseline electrical information was gathered in each PV ostium. A 28-mm Cryoballoon Advance (CB-A) (Arctic Front AdvanceTM, Medtronic©) was advanced, inflated, and positioned at each PV ostium. Optimal vessel occlusion was defined by selective contrast injection showing total contrast retention with no backflow into the left atrium. The ablation sequence in the first 50 patient was treating the left superior PV (LSPV) first, followed by the left inferior PV (LIPV), right inferior PV (RIPV), and right superior PV (RSPV). In the last 10 patients, the sequence was RSPV, RIPV, LIPV, and LSPV. Once vessel occlusion was deemed satisfactory, delivery of cryoenergy to allow freezing was commenced. Standard cryothermal applications lasted 180 s. Our target temperature was −40 °C within the first 60 s. If the temperature did not attain this value, an extra freeze was delivered. Successful PVI was defined as an absence of all PV potentials or their dissociation from an atrial activity. During the entire procedure, activated clotting time was maintained over 250 s by supplementing heparin infusion as required.
Prior to ablation of the right-sided PVs, a standard decapolar catheter was placed in the superior vena cava cranial to the RSPV, or in the right subclavian vein in order to pace the right phrenic nerve during ablation. Phrenic nerve pacing started once the temperature reached −20 °C in order to avoid balloon dislodgement due to diaphragmatic contraction in the first phase of cryoenergy application. Pacing was continued throughout the entire duration of cryoenergy delivery. In cases of phrenic nerve palsy, the freeze was immediately aborted with a "double stop" technique and recovery was observed. If recovery wasn't achieved in 15 minutes, the procedure was aborted and phrenic nerve was tested in the next day with "sniff test".
Post-procedural management
After completion of the procedure, the patients were continuously monitored via telemetry for at least 18 hours. Before discharge, a transthoracic echocardiogram was performed in all patients in order to exclude post-procedural complications. Patients were discharged on the following day and were instructed to continue AAD and anticoagulation therapy for at least 3 months.
Categorical variables are expressed as absolute and relative frequencies. Continuous variables were assessed for parametric distribution using Kolmogorov-Smirnov test. Continuous variables with parametric distribution were reported as mean ± standard deviation. Continuous variables with non-parametric distribution and discrete variables were reported as median and interquartile range. Correlations were assessed using Pearson's or Spearman's test, accordingly. Differences among all VR groups, including initial response and following each PV ablation, were assessed by repeated measures one-way ANOVA if all distributions were found parametric or Friedman's test if at least one distribution was found non-parametric. Differences between initial VR and VR after each PV ablation were assessed by paired Student's t test if distributions were found parametric or Wilcoxon matched-pairs test if at least one distribution was found non-parametric. A two-tailed p value of less than 0.05 was considered significant. All statistical analyses were performed with IBM SPSS Statistics for Windows, Version 24.0. (SPSS Inc., Chicago, IL, USA).
Patients were included from the 12th of March 2018 to the 7th of May 2018. No patient was excluded based on anatomical findings. Baseline clinical characteristics are shown in [Table 1].
Table 1. Baseline characteristics of the study population (n = 60)
|
N=60 |
| Age (years) |
59.37 +/- 8.57 |
| Male gender (%) |
36 (60) |
| Hypertension (%) |
29 (48) |
| Diabetes mellitus (%) |
12 (20) |
| Heart failure (%) |
4 (6) |
| Coronary artery disease (%) |
9 (15) |
| LVEF (%) |
57.43 ± 5.15 |
| LA diameter (mm) |
44.08 ± 4.85 |
LA = left atrium; LVEF = left ventricular ejection fraction.
Procedural characteristics
In all cases, all PVs were successfully isolated with the CB-A solely. The total procedural and fluoroscopy times were 73.8± 15.74 min and 21.01± 7.92 minutes, respectively.
Vagal Reactions Following Ablation in DistinctPulmonary Vein
The meanprobationn pause duration was 10251.83 ms ± 2826.23 m. .External cardiac vagalstimulation wass performed following each pulmonary vein ablation. In the first 50 patients after ablation in the LSPV, the mean pause was 8957.06 ± 2711.66 ms (p = 0.001). After ablation of the LIPV, RIPV and RSPV, the mean pause was 10017.36 ± 9127.0 ms (p = 0.88), 6020.16 ± 3780.709 ms (p < 0.001) and 1687.5±2183.7 ms (p < 0.001) respectively. The duration of the pause in response to ECVS significantly differed with respect to baseline after ablation in the LSPV -1367.553 ±2564.9 ms (p = 0.001), LIPV -214.222 ±9729.510 (p = 0.88), RIPV -4196.735 ±3725.82 ms (p < 0.001) and RSPV -8443.12 ±3656.0 ms(p < 0.001). Additionally, significant differences in pause duration were seen if comparing responses between LSPV and baseline -1367.55±2564.90 ms (p = 0.001), between LIPV and LSPV 1249.12 ±10209.55 (p = 0.42), between RIPV and LIPV-3922.67 ±10084.19 ms (p = 0.01) and between RSPV and RIPV -4312.29 ±4118.39 ms (p < 0.001).
Noteworthy, after the ablation of the RSPV, we noticed a significant reduction of vagal response to ECVS if compared to all other veins [Figure 1]. In order to confirm the hypothesis that the RSPV was responsible for an important acute VR reduction, due to the vicinity with the right superior ganglionated plexi and right inferior ganglionated plexi, in the last 10 patients the ablation procedure started in the RSPV. Interestingly, if starting with ablation in the RSPV, VR was reduced by 90.34%, 990.7 ± 379.78 ms (p < 0.001) if compared to baseline response.
We did not detect predictors of higher response to ECVS, both in the baseline clinical characteristics of the patient population, as age or sex (P = n.s.), nor in any procedural parameter.
Figure 1. Vagal Response to extracardiac vagal stimulation
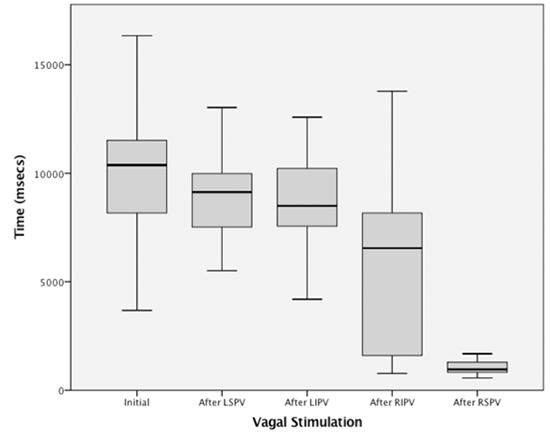
Vagal response to extracardiac vagal stimulation at the beginning and after each pulmonary vein ablation in the first 50 patients.
The ganglionated plexi, as well as the PV ostia, are richly innervated by both the sympathetic and parasympathetic autonomic systems [1,8].As described by Tolga et al, there is still no consensus among the authors on the anatomical location and number of the GPs. [9] A recent publication by our group showed that surprisingly the CB-ablation can modify acutely the parasympathetic tone during PVI. [10] Although ablation was performed only in the left atrium and not bi-atrial as reported by Pachon et al.[11] and Tolga et al.[12], in our case series acute modification of parasympathetic innervation was obtained in all patients. This might be explained by the extensive antral ablation created by the second generation cryoballoon, but this should not be accepted as a usual response. Because, in PVs with larger ostium, CB application will not cause antral ablation effect.
It has been shown that following CB application, large portion of the left atrium is ablated [13,14]. This extensive ablation in the LA and the modulation of the GPs might importantly contribute to the success of the CB-A, since the elimination or decrease of the VR might suggest an acute transmural lesion. Therefore, in order to improve outcomes in patients with AF, ablation of the GP has been proposed as an adjunctive complementary method to conventional PVI [15,16].
Anatomically, the cardiac nervous system can be subdivided into Extrinsic Cardiac Nervous System (ECNS), which contains fibers that mediate connections between the heart to the brain and spinal cord and the Intrinsic Cardiac Nervous System (ICNS), composed primarily by autonomic nervous fibers, which is an interconnected neural system consisting of epicardial ganglionated plexi and an extensive network of atrial intramural microganglia [17].
During ablation, parasympathetic, sympathetic and the sensory fibers are destroyed. The critical difference between them is that the parasympathetic postganglionic neuronal cells are found in the GPs [18] and in the cardiac wall [19]. Therefore, axons are short in length, and the ablation of these structures makes the parasympathetic reinnervation less probable, as the neuron body is eliminated [20]. This might enable long-term modulation of these ganglia from the endocardial surface [21].
On the other hand, the sensory and sympathetic postganglionic cells are far from the heart and are preserved whereas the sympathetic and sensory fibers eliminated by ablation have the capacity of recovery similar to that observed in post-transplantation patients [22].
A stepwise ECVS following ablation of each PV in the first 50 patients led to a producible reduction in VR [Figure 2].
Importantly, ablation in the RSPV produced the most impressive inhibitory responses to ECVS resulting in the vein producing the most marked loss of parasympathetic innervation. This might be explained by the proximity of 2 major GPs to the ostium of the RSPV and LA, the right superior ganglionated plexi and right inferior ganglionated plexi. The same region has the richest nerve density in comparison to the other PV-LA connection [23]. The CB-A wide antral ablation around this specific vein might largely include both GPs in the lesions' extension.
This observation is in accordance with finding of a previous study.In the latter, the authors compared the occurrence of spontaneous VR between 2 different strategies during CB-A procedure. The first consisted in starting ablation of left sided veins and successively approaching the septal PVs. In the second strategy, the operator approached the RSPV as first. Interestingly, if left sided veins were ablated first, spontaneous VR could be observed in 35.9 % patients. Conversely, only 1 patient out 42 experienced a VR in the other group. Of note, in this patient, ablation was stopped after 60 seconds due to right phrenic nerve injury [5].
The main difference between our study and the above mentioned paper by Myazaki and colleagues is that in our procedural protocol, VR reactions were voluntarily provoked by ECVS and therefore could be quantified in a standardized fashion.
The left lower GP is usually less richly innervated by parasympathetic fibers. In addition, if analysing anatomical findings, it is the farthest from the venous ostia of all. It usually is found at the inferior portion of the posterior wall of the left atrium, or>2cm away from the LIPV ostium [7,8,23]. These observations might explain the absence of significant changes after the ablation in the LIPV since the lesion might only partially reach the GP or not affect it at all [13].
Figure 2. Example of a vagal stimulation and cardiac parasympathetic modulation.

Initial vagal response to the extracardiac vagal stimulation before ablation and after each pulmonary vein ablation starting from the LSPV, LIPV, RIPV and RSPV. The interesting here is the gradual decrees of the sinus suppression to the extracardiac vagal stimulation.
Figure 3. The influence in the cardiac parasympathetic modulation after the right superior pulmonary vein ablation.
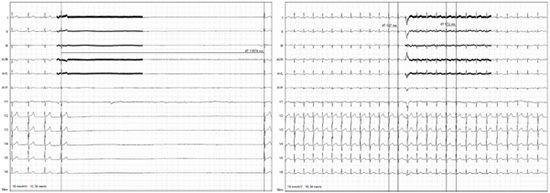
A vagal reaction to the extracardiac vagal stimulation before ablation (left ECG) and after solely the ablation of the right superior pulmonary vein (right ECG), the vagal response is almost abolished.
In this study, we solely stimulated the right vagal nerve causing sinus node suppression. Although both vagal nerves act on both the sinus node and the AV node, stimulation of the left vagal nerve produces a higher response on the AV node, whereas the stimulation on the right side produces a higher response on the sinus node. This study was conducted on a limited cohort of patients. Future studies enrolling larger patient populations are warranted in order to confirm our findings.
CdA receives compensation for teaching purposes and proctoring from AF solutions, Medtronic, Abbott, Biotronik, Atricure and research grants on behalf of the center from Biotronik, Medtronic, St Jude Medical Abbot, Livanova, Boston Scientific Biosense Webster.GBC receives compensation for teaching purposes and proctoring from AF solutions Medtronic and Biotronik.Pedro Brugada receives and speakers fees from Biotronik, Medtronic.