Unexplained and recurrent syncope represents a diagnostic challenge for cardiologists and electrophysiologists. It is known to affect quality of life, to cause physical injuries and to be a harbinger of sudden death. The current management1 suggests implantation of an ILR (Implantable Loop Recorder) in the presence of a normal ejection fraction, no or minimal structural heart disease, normal 12-lead ECG and negative first level work-up. Conversely, Electrophysiological Study (EPS) before implantation of an ILR is recommended only in the presence of sinus bradycardia and/or conduction disturbances on surface ECG. So far, the conduction disturbances liable of an EPS were the bundle branch block or the bifascicular block.2 EPS is a useful tool to detect atrio-ventricular conduction abnormalities, although with very low sensitivity.3,4,5,6,7 To overcome this limitation, class 1A and 1C drugs have been introduced into clinical practice.8,9,10,11,12
Ajmaline is a class 1A drug, a very powerful sodium channel blocker with relative short half-life.13 Its role in diagnostic testing is confined to two fields of application: to unmask the diagnostic electrocardiographic pattern of Brugada syndrome in the case of non-diagnostic basal ECG or as diagnostic testing to identify patients with paroxysmal atrio-ventricular blocks.8 It has a predominant extra-renal metabolism,13 thus it can be used with safety also in patients with advanced renal disease.14
In order to detect patients with paroxysmal AV block, ajmaline has been widely used in the past in subjects with surface ECG abnormalities, but standardized diagnostic values of His-Ventricular time are still missing.15,16,17,18,19,20,21 Another unanswered issue is the use of EPS with drug test in subjects with minor conduction abnormalities, as proposed in recent new diagnostic algorithms.22
So far, there is no data available in the literature about the role of the test in patients with minor or even without conduction disturbances on surface ECG.
Given these premises, we sought to evaluate the feasibility, utility, safety and diagnostic role of ajmaline challenge in unmasking the presence of an infrahisian disease in patients with recurrent and unexplained syncope, with preserved ejection fraction, regardless of the existence of conduction disturbances on surface ECG.
A total of 16 consecutive patients were enrolled in the study. Table 1 summarizes the baseline clinical characteristics of the population. Mean age was 76 ± 5 years (ranging from 68 to 86) and 7 were male (44%). All patients showed preserved left ventricular function on transthoracic echocardiogram, with a mean EF of 57 ± 5 %. Six patients (37%) had minimal structural heart disease (defined as the presence of mild valvular disease and/or mild left ventricular hypertrophy and/or mild dilatation of the aortic bulb). One patient had history of paroxysmal atrial fibrillation. All patients were in sinus rhythm at the time of enrolment and during the EPS. One patient had history of coronary artery disease and a coronary angiography excluded the progression of new significant disease. Nine patients (56%) had a conduction disturbance and were included in the group ECG+.
Table 1. Baseline clinical characteristics of study population (N = 16)
| Age (years), mean ± SD |
76 ± 5 |
| Males |
7 (44) |
| Associated structural heart diseases: |
|
| Any abnormality |
10 (62.5) |
| Ischemic |
1 (6.25) |
| Valvular |
5 (31) |
| Hypertensive |
2 (12.5) |
| Other |
2 (12.5) |
| LV ejection fraction (%), mean ± SD |
57 ± 5 |
| ECG conduction disturbances |
9 (56) |
| Sinus Rhythm at EPS |
16 (100) |
| History of paroxysmal/persistent AF |
1 (6.25) |
Data are expressed as No. (%) unless otherwise specified
Table 2 shows the type of conduction disturbances on 12-leads ECG found in this group of patients. The most common was the first degree AV block associated with the left bundle branch block (3 patients, corresponding to 33%). Two patients (22%) presented with isolated right bundle branch block. There was a patient with isolated left bundle branch block and two patients with two kind of bifascicular block, respectively: one with first degree AV block associated to left anterior fascicular block and one patient with left bundle branch block. An isolated first degree AV block was present only in one patient.
Table 2. Type of conduction disturbances on surface ECG in the group ECG+ (PR interval ≥ 200 msec and/or QRS duration > 100 msec)
| First degree AV Block |
1 (11.1) |
| RBBB |
2 (22.2) |
| LBBB |
1 (11.1) |
| First degree AV block + LAFB |
1 (11.1) |
| RBBB + LAFB |
1 (11.1) |
| First degree AV block + LBBB |
3 (33.3) |
Data are expressed as No. (%), RBBB = Right Bundle Branch Block, LBBB = Left Bundle Branch Block, LAFB = Left anterior fascicular block
Seven patients (44%) had no conduction disturbance on surface 12-leads ECG and were included in the group ECG-.
Table 3 highlights the baseline clinical characteristics of the two groups. They did not differ for the mean age (75 ± 6 years and 76 ± 5 years, P=0.96) and the mean ejection fraction (57 ± 4% and 59 ± 2%, P=0.18).
Table 3. Baseline characteristics in the group with (ECG +, N = 9) or without (ECG -, N = 7) conduction abnormalities on 12-leads ECG
|
ECG + (n = 9) |
ECG – (n = 7) |
P-value |
| Age (years), mean ± SD |
75 ± 6 |
76 ± 5 |
0.96 |
| Males |
6 (67) |
1 (14) |
0.06 |
| Associated structural heart diseases: |
|
|
|
| Any abnormality |
5 (56) |
5 (71) |
|
| Ischemic |
0 (0) |
1 (14) |
|
| Valvular |
3 (33) |
2 (29) |
|
| Hypertensive |
1 (11) |
1 (14) |
|
| Other |
1 (11) |
1 (14) |
|
| LV ejection fraction (%), mean ± SD |
57 ± 4 |
59 ± 2 |
0.18 |
| ECG conduction disturbances |
9 (100) |
0 (0) |
|
| QRS duration (msec), mean ± SD |
133 ± 30 |
90 ± 7 |
0.0037 |
| PR interval (msec), mean ± SD |
234 ± 79 |
174 ± 22 |
0.07 |
Data are expressed as No. (%) unless otherwise specified
Males were more likely to have a conduction disturbance on surface ECG, although the difference was not statistically significant (P=0.06).
Mean QRS duration was significantly different between the two groups (133 ± 30 msec and 90 ± 7 msec, P <0.01) while there was a trend toward a difference in the PR interval duration (234 ± 79 msec and 174 ± 22 msec) though it did not reach a statistical difference (P= 0.07).
All 16 patients underwent the basal EPS (figure 2 and table 4). No patient had abnormal cSNRT (group ECG+ 372 ± 140 msec, group ECG– 365 ±151 msec, P=0.67) or developed intra or infrahisian block during incremental atrial pacing. All patients showed a normal response after atrial and ventricular programmed electrical stimulation. AH intervals were statistically different between the groups: mean AH intervals in group ECG+ were 155 ± 58 msec while they were 86 ± 16 msec in group ECG- (P=0.02). Basal mean HV intervals were statistically different between the two groups: they were 68 ± 12 msec in group ECG+ and 56 ± 7 msec in group ECG- (P=0.036).
Figure 2. Results
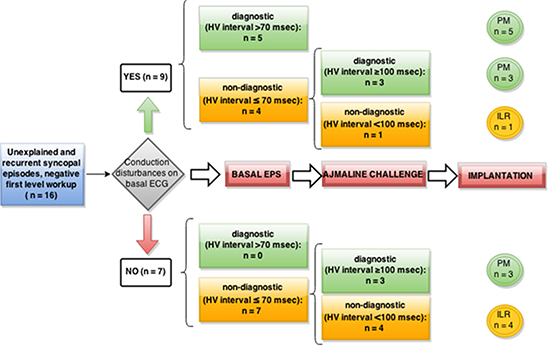
Table 5 summarizes the comparison of the results of diagnostic basal HV interval between the two groups. In the group ECG+, 5 patients (56%) had a basal diagnostic HV interval with a mean value of 76 ± 6 msec, while 4 patients (44%) had a non-diagnostic HV interval (58 ± 8 msec). The difference between this baseline values reached a significant statistical difference (P < 0.01).
Table 4. Parameters at basal EPS (N = 16)
| BASAL EPS |
ECG + (n = 9) |
ECG – (n = 7) |
P-value |
| cSNRT (msec) |
372 ± 140 |
365 ± 151 |
0.67 |
| AH (msec) |
155 ± 68 |
86 ± 16 |
0.02 |
| HV (msec) |
68 ± 12 |
56 ± 7 |
0.036 |
Data are expressed as mean ± SD, unless otherwise specified
In the group ECG-, none had a diagnostic basal HV interval, with a mean value of 56 ± 7 msec. Of note, these values were not statistically different from those registered in the group ECG+ with non-diagnostic basal HV interval (P=0.74).
Response To Ajmaline Challenge And Side Effects
Eleven patients, of which 4 in the group ECG+ and 7 in the group ECG-, underwent drug test with ajmaline. All patients were tested with the maximal dose required to complete the challenge, and there was no premature interruption of the drug infusion. No side effects were recorded during drug administration. Of the four patients in the group ECG +, 3 (75%) developed a diagnostic interval with a mean HV of 108 ± 2 msec (Table 5). In the group ECG -, three patients (43%) showed a diagnostic HV interval, with a mean value 108 ± 8 msec. It is noteworthy that the mean maximum value of HV interval reached during a positive challenge is not statistically different between the two groups (P=0.89).
Table 5. Comparison of basal HV interval (A) and stress HV interval (B)
| Basal HV interval |
ECG + |
ECG – |
P-value |
| DIAGNOSTIC (N = 5) |
76 ± 6 msec |
- |
|
| NON-DIAGNOSTIC (N = 4+7) |
58 ± 8 msec |
56 ± 7 msec |
0.74 |
| Stress HV interval |
ECG + |
ECG – |
P-value |
| DIAGNOSTIC (N = 3+3) |
108 ± 2 msec |
108 ± 8 msec |
0.89 |
| NON-DIAGNOSTIC (1+4) |
75 ± 0 msec |
80 ± 6 msec |
- |
Data are expressed as mean ± SD
Finally, when properly evaluable, no patients developed a Brugada type 1 on right precordial leads during the test.
After the protocol application (EPS + drug challenge), a total of eleven patients (69%) were implanted with a permanent pacemaker while five patients (31%) underwent an ILR implantation.
Among the patients implanted with a PM: 8 belonged to the group ECG +, of which 5 after a basal EPS and 3 after the drug challenge; and 3 belonged to the group ECG-. The protocol unmasked an infrahisian disease in 89% of patients with ECG+ and in 43% of patients in group ECG-. Finally, five patients were implanted with a ILR (31%): 1 in the group ECG+ and 4 in the group ECG-.
Patient implanted with a pacemaker received appropriate devices for their conditions. Some patients in the group ECG+ and all patients in the group ECG- were implanted with pacemakers equipped with algorithms aimed at reducing the ventricular pacing percentage, such as the Managed Ventricular Pacing26 and the SafeR.27 In the latter case, it is possible to review retrospectively, into pacemaker memory, all the block types for which ventricular pacing is activated.
A mean follow up of 13 ± 3 months was available for all patients. Follow-up was not statistically different among the two groups (P=0.85). Patients in the group ECG+ had no recurrence of syncopal episodes and one patient died because of a cerebral neoplasia.
In the group ECG – there was no recurrence of syncope in any patient. One of them showed, on ILR memory, an asymptomatic episode of two to one AV block and was consequently implanted with a permanent pacemaker.
Analysis of stored pacemaker data in patients implanted in both groups demonstrated the occurrence of various types of paroxysmal AV block (type 2, advanced and complete AV block). In particular, among the patients belonging to the group ECG-, the retrospective analysis of the EGM stored into pacemaker memory showed that all of them (n = 3, 100%) had the occurrence of the above mentioned types of AV block, with regular activation of ventricular pacing back-up algorithms.
To the best of our knowledge, this is the first report of the use of ajmaline challenge in unmasking the presence of an infrahisian disease in patients with recurrent and unexplained syncope, preserved ejection fraction and no conduction disturbances on surface ECG.
The use of drug stress test during EPS in current guidelines1 is a class IIb level B indication in patients with 12-lead ECG bundle branch block, when non-invasive tests failed to make the diagnosis. In patients with normal ECG, no structural heart disease and no palpitations, EPS is a Class III Level B indication. However, very recently, Rosanio et al15 proposed a diagnostic algorithm according to which the presence of a Type 1 AV block can be considered an indication to perform EPS. Consequently, it can be noticed a trend toward a theoretical extension of the use of the EPS. However, nowadays only 2% of patients with unexplained syncope assessed by cardiologists undergo to EPS, and even fewer if they are evaluated by other specialists.1,28
Another thorny issue is represented by the lack of standardized diagnostic values of HV time during a basal EPS or after a drug stress test.15,16,17,18,19,20,21 Moreover, some of these studies were conducted before the era of primary prevention of sudden cardiac death, and consequently patients with left ventricular dysfunction were included. Enormous clarity and great strides have been made in the ISSUE Study,29 where Moya and colleagues enrolled patients with unexplained syncope after a complete negative workup, including an EPS. Patients were implanted with an ILR and divided into four groups according to their basal condition: syncope alone, syncope alone and positive tilt test, syncope associated to bundle branch block and negative EPS and, at last, patients with structural heart disease and negative EPS. The group with bundle branch block and negative EPS4 consisted of 52 patients. Criteria to consider diagnostic the EPS were a basal HV interval ≥ 70 msec and the development of 2nd or 3rd degree infrahisian block after ajmaline infusion. During the follow-up authors recorded 21 asystolic pauses, of which 17 were AV blocks and four were sinus pauses. This means that 1/3 of patients were false negative at EPS, as expected by the low sensitivity of the exam but also taking into account the high specific values considered in that study. Still in the ISSUE study, if we consider the group of isolate syncope and the tilt positive group,30 only 66% of patients had undergone an EPS. After a mean follow-up of 9 ± 5 and 10 ± 5 months, of the 16 asystolic pauses detected, 14 were sinus arrests and only 2 (1.8%) were AV blocks. Here EPS seems to be more sensitive than the third group, especially towards the AV block. But it has to be kept in mind that only 2/3 of patient underwent an EPS with the aforementioned criteria of positivity.
In a recent study,31 Conte and colleagues used ajmaline challenge in elderly patients to unmask atrio-ventricular conduction disease and/or the typical Brugada ECG pattern. No values of basal HV interval to be considered diagnostic for conduction disease are reported. After ajmaline infusion they considered a response abnormal only when the prolongation of HV exceeded 100 msec.
In our study, the application of the protocol with less severe diagnostic criteria during ajmaline challenge, ensured a prompt diagnosis in the group ECG+ in 8 over 9 patients (89%). With the same criteria, in 3 over 7 patients (43%) in the group of patients with normal ECG, a diagnosis was reached. The instrumental follow-up at pacemaker interrogation, with events of various kinds of paroxysmal AV block stored, including complete AV block, demonstrates that the mechanism of the syncopal episodes occurring before EPS and PM implantation were cardiogenic and caused by severe brady-arrhythmias. Although the very small population studied in the group ECG-, no false positives emerged during the follow-up.
As expected, the sensitivity of the EPS without ajmaline was very low in patients with ECG conduction abnormalities. The use of ajmaline significantly improved the sensitivity of the EPS in this group. This is in line with what has been described previously.3,4,5,6,7 Fujimura and colleagues3 reported that sensitivity of basal EPS is 37.5% in patients with paroxysmal sinus pause and 15.4% in patients with paroxysmal AV block. The introduction of class 1A and 1C agents during EPS improves sensitivity of the test up to 50-80%.10 However, we intentionally included in the group ECG+ patients with any conduction abnormality on surface ECG. According to our inclusion criteria, we studied some patients that, considering the last guidelines, would have directly implanted an ILR. In the light of this result, it seems that the sensitivity reported here is higher than that reported up to now in the literature, and it exceeds 95%. In fact, in the group ECG+, the only patient implanted with an ILR showed an isolated PR prolongation on surface ECG.
The results in patients without any conduction disorder (ECG -) are rather surprising. First of all, the sensitivity of the EPS without ajmaline verges on zero. Ajmaline helps improving the sensitivity and unmasks the presence of an infrahisian disease, which could not have been proved in any other way. Furthermore, the most surprising result is that the mean maximum value of HV interval reached during a positive ajmaline challenge is not statistically different between this group of patients and that registered in the group ECG+. In other words, it seems to be independent of the presence of a conduction disturbance on surface ECG.
These findings allow us to speculate that diagnostic HV interval values considered here are provided with sufficient sensitivity and specificity, but further studies with larger population are required to support this speculation.
One possible explanation of our results was the selection during the anamnesis, with considerable attention to the clinical features of syncopal episodes. We enrolled patients with two or more syncopal episodes per year, or patients with a single episode but with physical injury. In both cases, and with the limits and difficulties often correlated with anamnesis, it was assumed that with some specific clinical features, the syncope was of cardiogenic nature.
Furthermore, we are aware that the diagnostic role of this test is highly dependent on the basis of the clinical features of syncopal episodes.23 In fact, from a clinical point of view, we found that the presence of a previous history of injury secondary to syncope and patients of female sex were more likely to have a positive result and therefore to implant a pacemaker, regardless of the presence of ECG conduction disturbance. This findings confirm those of a recent retrospective study.32 Ahmed and colleagues studied the clinical predictors of pacemaker implantation in 200 patients suffering from unexplained syncope receiving an ILR. Of the 33 patients with clinical significant bradycardia requiring PM implantation, history of injury secondary to syncope was found to be the strongest independent predictor for PM implantation, regardless of the presence of 12-lead ECG conduction abnormalities. Female sex was another strong predictor, but only in patients with ECG conduction disturbances.
Despite in the ISSUE study30 only 1% of patients experienced a severe injury due to syncopal relapse, a potential advantage of EPS in this setting is to unmask infrahisian disease, avoiding the implantation of an ILR and thus the traumatic consequences of syncope recurrence.
In our study, ajmaline challenge proved to be a safe procedure. Ajmaline has a very rapid effect, usually in the first 2-3 minutes after the end of infusion. Pharmacokinetics studies13 show that the duration of electrophysiological effects is short (about 30 minutes), in comparison with the slow decay of plasma concentrations (half-life of 7.3 ± 3.6 hours), so that it is believed that a threshold concentration exists under which no drug effect can be detected. We did not record any ventricular arrhythmias during the drug challenge nor any transient second or third degree AV block. Nevertheless, ajmaline infusion has to be performed in an appropriate environment, with advanced life-support facilities available, as external defibrillator and ventricular back-up pacing.
This study has several limitations. First, this is a monocentric observational study. Second, the study population is too small to draw final conclusions. Therefore, the present study can be considered only as preliminary.