A Case of Wide Complex Tachycardia in a Patient with a Biventricular Assist Device
Abrams, Mark P, Whang, William, Iyer, Vivek, Garan, Hasan, Biviano, Angelo
1NewYork Presbyterian Hospital – Columbia University Medical Center, Department of Medicine , 177 Fort Washington Ave New York.
This case report highlights the variety of wide complex tachycardias, and the need for their prompt management, in the growing population of patients with circulatory support devices. We present a case that demonstrates how a wide complex supraventricular tachycardia in a patient with a biventricular assist device can be safely and effectively targeted for treatment using percutaneous radiofrequency catheter ablation, allowing for clinical improvement, weaning of RVAD treatment, and discharge home with LVAD alone.
Key Words : Vad, Arrhythmia, Ablation, Tachycardia, Atrial Flutter, Atrial Fibrillation.
Correspondence to: Angelo Biviano,
177 Fort Washington Ave
Milstein 5th Floor, Room 5-435F
New York, NY 10032
With the increasing use of ventricular assist devices (VAD) as a bridge to transplant or as destination therapy, there have been more reports of the presence and implications of arrhythmias associated with such devices. This case report illustrates that although patients with underlying heart failure requiring VADs may have a high pretest probability of having ventricular tachycardia and ventricular fibrillation, one must also consider other etiologies for wide complex tachycardias, including supraventricular arrthythmias in the presence of baseline bundle branch block or rate-related aberration.
A 54 year old man with a remote history of Hodgkin’s lymphoma, treated with splenectomy and radiation in 1986, was transferred from an outside hospital for further management of acute cardiogenic shock. He initially presented to his primary doctor with chest pain and had an electrocardiogram (ECG) with anterior ST elevations concerning for acute myocardial infarction. He underwent coronary catheterization at the outside hospital, which showed a complete occlusion of the proximal left anterior descending artery as well as an unspecified circumflex artery lesion. During balloon angioplasty, the patient became hemodynamically unstable. The procedure was aborted and an intra-aortic balloon pump (IABP) was placed. At this time, he was transferred to our medical center’s cardiac intensive care unit for further management.
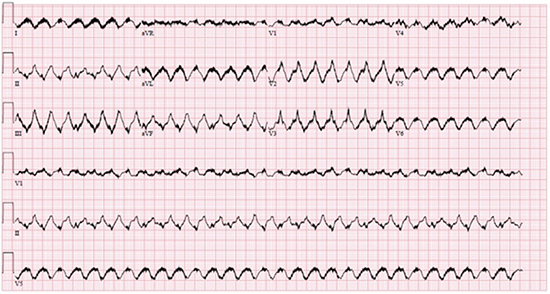
Because of the severely reduced biventricular function and refractory cardiogenic shock despite the presence of an IABP, a biventricular assist device (BiVAD) was implanted. His post-operative course was complicated by acute renal failure requiring continuous veno-venous hemodialysis. He was also noted to have several episodes of wide complex tachycardias in the setting of a baseline non-specific intraventricular conduction delay. Several arrhythmias were identified, including ventricular tachycardia (VT) and ventricular fibrillation (VF) (see Figure 1), as well as atrial flutter with varying amounts of AV block (Figure 2). The patient was treated with esmolol, amiodarone, procainamide, and lidocaine for these arrthythmia. However, the patient continued to manifest one predominant wide complex tachycardia that complicated attempts to wean the patient from a BiVAD to a left ventricular assist device (LVAD) alone (Figure 3, left panel). Therefore, an electrophysiology study (EPS) and radiofrequency ablation was performed with the goal of stabilizing rhythm control and optimizing hemodynamic management.
Figure 1A. Baseline ECG Baseline 12-lead ECG showing normal sinus rhythm, right bundle branch block, and evidence of an extensive anterior myocardial infarction
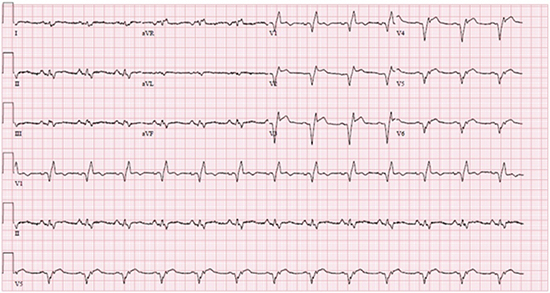
Figure 1B. Ventricular Fibrillation. 12-lead ECG showing a polymorphic wide complex tachycardia consistent with coarse ventricular fibrillation. The artifact present is secondary to electrical interference from a normally functioning VAD
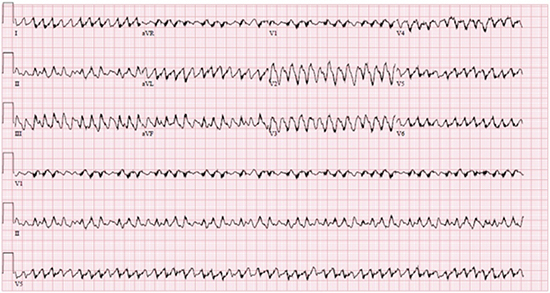
Figure 1C. Ventricular Tachycardia. 12-lead ECG noting a wide complex tachycardia with rapid ventricular conduction and a profound axis shift from baseline, most consistent with ventricular tachycardia. The artifact present is secondary to electrical interference from a normally functioning VAD
Despite more pronounced AV block during previous episodes of atrial flutter (Figure 2), at EPS the arrhythmia was diagnosed as cavotricuspid isthmus-dependent atrial flutter with 2:1 conduction to the ventricle (Figure 3). During radiofrequency ablation to the cavotricuspid isthmus (CTI), the arrhythmia terminated to sinus rhythm. Moreover, further programmed ventricular stimulation did not result in inducible VT. After the atrial flutter ablation, the patient was maintained on oral amiodarone and metoprolol and did not have recurrence of any significant tachycardia through hospital discharge three weeks post-ablation. After sustained restoration of sinus rhythm and improvement in right-sided hemodynamics, the patient’s right ventricular level of support was weaned, allowing for the right ventricular assist device (RVAD) circuit to be explanted and the patient to be discharged home with destination LVAD therapy.
Figure 2. 12-lead ECG noting a wide complex tachycardia with variable AV block and intermittent ventricular pacing allowing for visualization of atrial flutter waves. The QRS complexes are similar to that of baseline, including RBBB and Q-waves in anterior leads. The artifact present is secondary to electrical interference from a normally functioning VAD
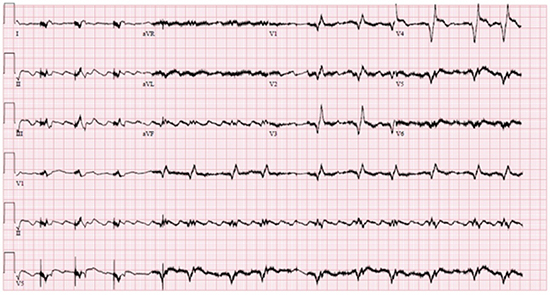
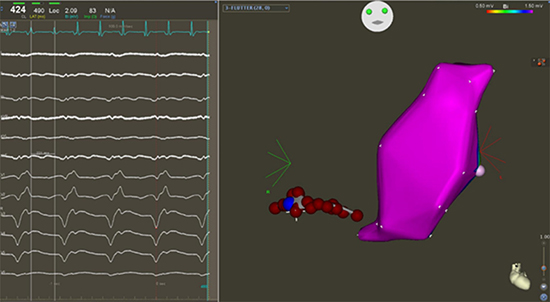
Figure 3. CTI and Right Ventricular Mapping. The left panel shows electrograms demonstrating 2:1 atrial flutter with a cycle length of 424 msec. The artifact present is secondary to electrical interference from a normally functioning VAD. The right panel is a left anterior oblique (LAO) projection of the ablation lesions along the CTI line as well as the right ventricle map, which is free of scar
This case report highlights that even in patients with a high pretest probability of having VT/VF, it is important to consider other known causes of wide complex tachycardias that can contribute toward hemodynamic compromise. Studies have shown that patients with severe heart failure requiring VADs were more likely to have ventricular arrhythmias that negatively impacted survival and other outcomes.1 Nevertheless, it has also been demonstrated that atrial arrhythmias are fairly common in patients with VADs and have affected outcomes including mortality by a variety of proposed mechanisms.2,3 This case illustrated that in patients with VADs, the treatment not only of ventricular arrhythmias but also of supraventricular arrhythmias is important for longer term management, as ablation of the atrial flutter allowed for RVAD explantation and discharge home with destination LVAD.
The main etiologies of a wide complex tachycardia may include ventricular arrhythmias, supraventricular arrhythmias in the setting of underlying bundle branch block/intraventricular conduction defect or with rate-related aberrancy, or supraventricular arrhythmias with ventricular pre-excitation. While certain non-invasive diagnostic algorithms for distinguishing between ventricular or supraventricular sources of the arrhythmia have been suggested historically and reviewed more recently, there is still much inter-user variability among the algorithms, making them somewhat unreliable especially in the context of regular wide complex tachycardias.4,5 Furthermore, their utility in LVAD patients has not been established. The use of EPS to diagnose the arrhythmia is more invasive, but also provides definitive information as well as the potential for immediate and effective treatment with ablation. Since EPS has been demonstrated to be safe in patients with VADs and can produce excellent results regardless of the etiology of the arrhythmia, it should be considered a safe adjunct or alternative to oral and parenteral antiarrhythmic treatments.
Patients with VADs can tolerate wide complex tachycardias including ventricular tachyarrhythmias more effectively from a hemodynamic standpoint. However, a known common presentation of ventricular arrhythmias is not sudden death, but rather acutely worsening right heart failure.6 Catheter ablation of ventricular arrhythmias has been shown to be safe in patients with VADs and can result in decreased symptoms and burden of antiarrhythmic medications.7,8 Nevertheless, atrial arrhythmias have previously been shown to be prevalent in patients with VADs with resultant increased signs and symptoms of right heart failure.2 We show in this case that effective control of atrial arrhythmias helped permit recovery of this patient’s right ventricular function and ultimately allowed for explantation of the RVAD and discharge from the hospital.
As the use of mechanical assist devices for heart failure continues to expand, there remains much to be studied about the impact these devices have on arrhythmia prevalence and patient outcomes, and vice versa. This case demonstrates that: (i) VAD patients can sustain multiple wide complex tachycardias of different etiologies, including ventricular tachycardia, ventricular fibrillation, and supraventricular tachycardias such as atrial flutter with baseline intraventricular conduction defect or rate-related aberration; (ii) electrophysiology study and radiofrequency ablation of clinically deleterious wide complex tachycardias in VAD patients, including supraventricular tachycardias with rapid ventricular response, are possible and effective for rhythm control and can facilitate recovery and overall clinical outcome. In summary, consideration of supraventricular tachycardias in VAD patients with medically refractory wide complex tachycardias allows for relatively straightforward diagnosis and management with ablation, resulting in a significantly positive impact upon a patient’s clinical course.